Drug-Induced Pancreatitis Risk Checker
Medication Risk Assessment
Select any medications you're currently taking. This tool identifies high-risk drugs linked to severe pancreatitis.
Risk Assessment Results
When you take a medication, you expect relief - not a life-threatening reaction. But for some, a common drug can trigger severe pancreatitis, a sudden and dangerous inflammation of the pancreas. Unlike gallstones or alcohol, which are more familiar causes, drug-induced pancreatitis flies under the radar. It doesn’t always show up right away. It might take weeks. And when it does, it can be mistaken for indigestion or a stomach bug. By the time it’s caught, it’s often too late. The good news? If you know the signs and act fast, you can stop it before it destroys your pancreas.
What Is Drug-Induced Severe Pancreatitis?
Severe pancreatitis from medication happens when a drug damages the pancreas, causing it to swell, leak digestive enzymes, and start digesting itself. This isn’t rare - about 1 in 30 acute pancreatitis cases comes from a medication. But because doctors don’t always think of it, patients often wait days or weeks before getting the right tests. The condition is called severe when it leads to organ failure, tissue death (necrosis), or a body-wide inflammatory response. Mortality rates hit 15-30% in these cases, higher than with gallstone-related pancreatitis. The key difference? With drug-induced pancreatitis, stopping the medicine can reverse the damage. That’s why early recognition saves lives.
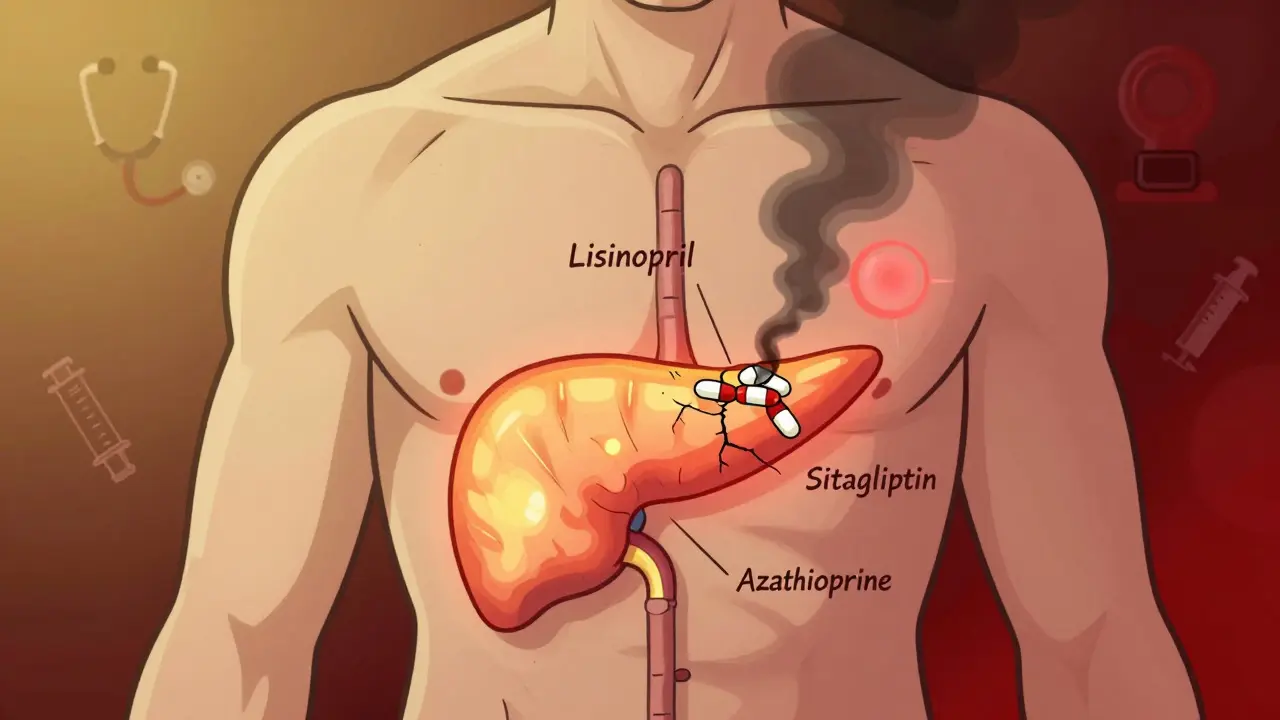
Which Medications Carry the Highest Risk?
Not all drugs cause this. But eight classes have strong, well-documented links. If you’re taking any of these, pay attention:
- ACE inhibitors - especially lisinopril and enalapril. These are common for high blood pressure, but they’ve triggered pancreatitis in patients after months or even years of use.
- Diuretics - furosemide (Lasix) and hydrochlorothiazide. These are often prescribed for fluid retention and hypertension.
- Diabetes drugs - exenatide (Byetta), sitagliptin (Januvia), and SGLT2 inhibitors like dapagliflozin. The FDA added stronger warnings to these in 2023 after a surge in reports.
- Statins - simvastatin and atorvastatin. Even long-term users can suddenly develop pancreatitis. One case reported lipase levels over 2,800 after three years on simvastatin.
- Immunosuppressants - azathioprine and valproic acid. These carry the highest risk of necrosis. Azathioprine causes severe pancreatitis in up to 18% of users, and valproic acid in 22%.
- Antiretrovirals - particularly didanosine, used in HIV treatment.
- Oral contraceptives - those with ethinyl estradiol.
It’s not about the dose. It’s about your body’s reaction. Some people take these drugs for years without issue. Others develop pancreatitis after just one or two doses. That’s why timing matters more than quantity.
Warning Signs You Can’t Ignore
These symptoms don’t always come with a warning label. But if you’re on one of the high-risk meds and notice any of these, don’t wait:
- Intense, constant upper abdominal pain - often radiating to your back. It doesn’t come and go. It stays. And it’s worse after eating.
- Pain that wakes you up at night - this is a red flag. Most stomach issues don’t disrupt sleep.
- Nausea and vomiting - especially if it’s persistent and not relieved by over-the-counter meds.
- Fever or rapid heartbeat - signs your body is in full inflammatory mode.
- Jaundice (yellowing of skin or eyes) - if the inflammation blocks bile ducts.
One patient on Reddit described it this way: “It felt like someone was stabbing me behind my ribs and twisting the knife.” That’s not normal indigestion. That’s your pancreas dying.
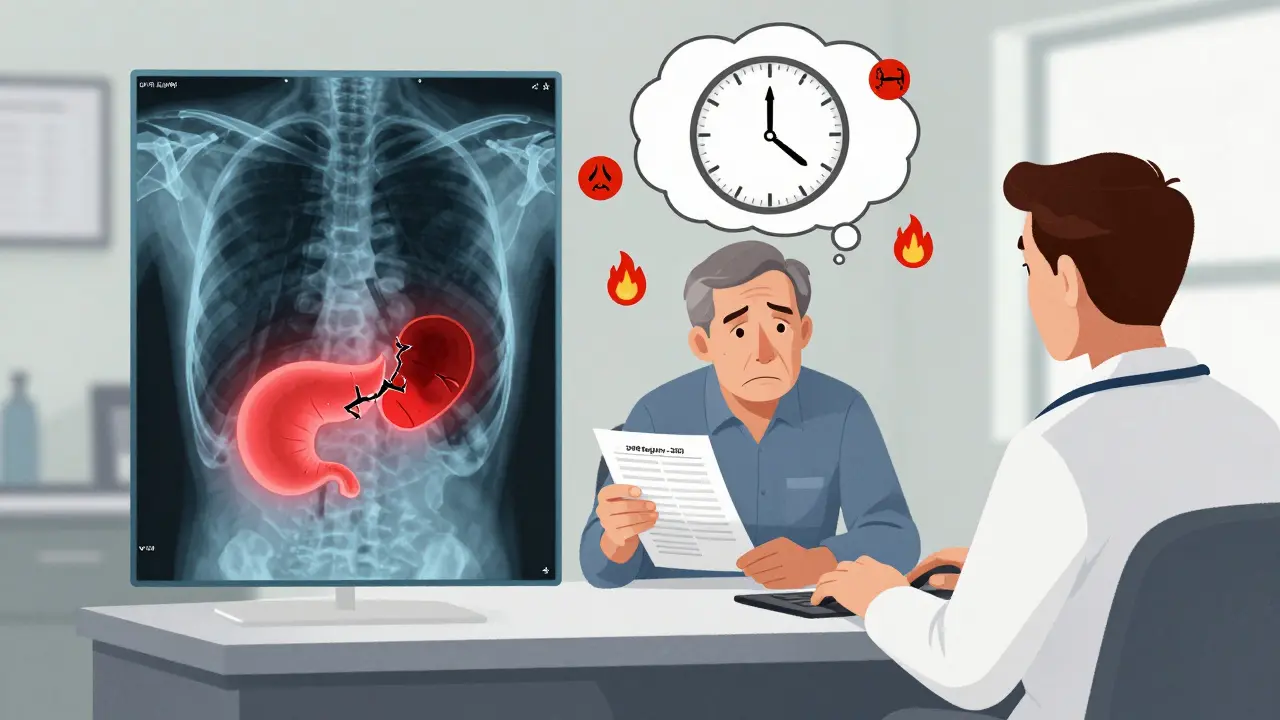
How Doctors Diagnose It
There’s no single test. Diagnosis relies on three things:
- High lipase levels - at least three times above normal. Lipase is more accurate than amylase for pancreatitis.
- Imaging - a CT scan shows swelling, fluid, or dead tissue (necrosis). If more than 30% of the pancreas is damaged, it’s classified as severe.
- Timing - symptoms appeared within 4 weeks of starting the drug and improved after stopping it. This is the gold standard for linking cause and effect.
Rechallenge - restarting the drug to see if symptoms return - is the only way to prove it definitively. But doctors rarely do it. Why? Because it’s dangerous. If you had severe pancreatitis once, doing it again could kill you.
What Happens in the Hospital
If you’re diagnosed with severe drug-induced pancreatitis, treatment starts immediately:
- Stop the drug - within 24 hours. Delaying increases complications by 37%.
- IV fluids - 250-500 mL per hour for the first 24-48 hours. This keeps blood flowing to the pancreas and prevents organ failure.
- Pain control - acetaminophen first. If that’s not enough, low-dose morphine. Avoid NSAIDs like ibuprofen - they can worsen kidney stress.
- Feeding - you’ll be NPO (nothing by mouth) at first. But within 48 hours, if you can’t eat, a feeding tube goes in through your nose to your small intestine. You need calories to heal.
- Antibiotics - only if the pancreas tissue becomes infected. Otherwise, they do more harm than good.
One study found patients who got early enteral feeding recovered 40% faster than those who stayed on IV nutrition too long. Nutrition isn’t optional - it’s part of the cure.
Why This Is Often Missed
Doctors aren’t ignoring you. They’re trained to think of gallstones first - they cause 40% of cases. Then alcohol. Then genetics. Medications? They’re an afterthought. A 2023 survey of ER physicians found only 23% routinely asked about drug use when a patient presented with abdominal pain. That’s dangerous. One patient on HealthUnlocked wrote: “My rheumatologist called my pain ‘just gastritis’ while I was on azathioprine. By the time they scanned me, I had 40% necrosis. I spent three weeks in the ICU.”
Also, the delay between taking the drug and getting sick makes it harder to connect the dots. Someone on lisinopril for five years might not think it’s the culprit. But that’s exactly when it happens - after long-term use.
What You Should Do Now
If you’re on one of the high-risk medications listed above, here’s what to do:
- Know your risk - if you’re over 60, taking five or more medications, or have a history of pancreatitis, your risk is higher.
- Track your symptoms - if you get new, persistent abdominal pain, write down when it started and what meds you’re on.
- Ask for a lipase test - don’t wait for a CT scan. Ask your doctor to check your lipase level. It’s cheap, fast, and tells you everything.
- Don’t stop medication on your own - especially if it’s for blood pressure, diabetes, or autoimmune disease. Talk to your doctor. They may switch you to a safer alternative.
One 45-year-old woman on lisinopril had lipase levels at 1,250 (normal is under 60). She was hospitalized for five days. After stopping the drug, she’s been pain-free for two years. That’s the power of catching it early.
What’s Changing in 2026
The medical world is waking up. The FDA now requires stronger warnings for SGLT2 inhibitors. The NIH launched the Drug-Induced Pancreatitis Registry (DIPR) in January 2023 - it’s already tracked over 300 cases. Hospitals in the U.S. are now using automated alerts in electronic records to flag patients on high-risk drugs. And insurance companies? They’re denying reimbursement for severe pancreatitis cases they consider preventable. That’s pushing hospitals to act.
But the biggest change is in awareness. More doctors are asking about medications. More patients are speaking up. And that’s saving lives.
Long-Term Outlook
If caught early and the drug is stopped, most people recover fully. No permanent damage. No chronic pancreatitis. No lifelong pain. But if you wait - if you ignore the pain or assume it’s just gas - the damage can be irreversible. Pancreatic necrosis can lead to infection, sepsis, and organ failure. That’s why timing is everything.
There’s no cure for severe pancreatitis. But there is a prevention: awareness. Knowledge. And asking the right question - Could this be the medicine?