Introduction to Heparin Sodium Storage and Handling
As a healthcare provider, it is crucial to understand the best practices for storing and handling heparin sodium, an essential anticoagulant medication used in various clinical settings. This article will provide you with valuable information and tips on how to properly store and handle heparin sodium, ensuring its efficiency, safety, and effectiveness for your patients. Let's dive into the details and explore the following ten sections:
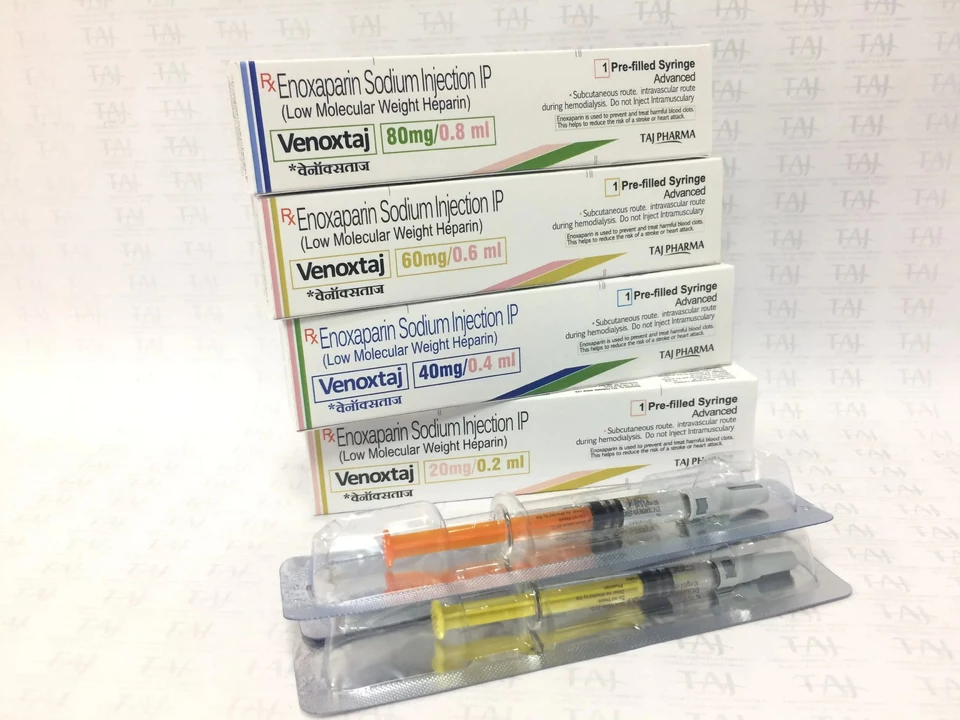
Understanding Heparin Sodium and Its Uses
Before we delve into the best practices for storage and handling, it is essential to understand what heparin sodium is and its uses. Heparin sodium is an anticoagulant medication derived from animal tissues, primarily used to prevent and treat blood clots in various medical conditions such as deep vein thrombosis, pulmonary embolism, and during surgical procedures. As a healthcare provider, you must be well-versed in the indications and contraindications of heparin sodium to ensure the safety and well-being of your patients.
Proper Storage Conditions for Heparin Sodium
Proper storage conditions are vital to maintaining the potency and stability of heparin sodium. It should be stored at room temperature, between 20°C to 25°C (68°F to 77°F), and away from direct light and heat sources. Additionally, it is crucial to keep heparin sodium in its original container, which is designed to protect the medication from light and moisture. Always check the expiration date before administering heparin sodium, and discard any expired medication appropriately.
Handling Heparin Sodium Vials
Handling heparin sodium vials requires care and attention to avoid contamination and ensure accurate dosing. Always use aseptic techniques when handling vials, such as wearing gloves and using alcohol swabs to clean the vial's rubber stopper. When withdrawing heparin sodium from a vial, use a sterile needle and syringe, and avoid touching the needle to any non-sterile surfaces. Following these precautions will help maintain the medication's sterility and protect your patients from potential infections.
Preparing Heparin Sodium Infusions
When preparing heparin sodium infusions, it is important to use the appropriate diluent, as specified by the manufacturer, to ensure proper concentration and stability. Once heparin sodium has been diluted and prepared for infusion, it should be administered promptly, as the stability of the solution decreases over time. Additionally, take care to avoid any air bubbles in the infusion line, as these can lead to inaccurate dosing and potential complications for your patients.
Administering Heparin Sodium Injections
Administering heparin sodium injections requires precision and care to ensure patient safety and comfort. When administering subcutaneous injections, always choose an appropriate injection site, such as the abdomen or thigh, and alternate sites to minimize tissue damage. Inject the medication slowly and carefully, and do not massage the injection site, as this can cause bruising and affect the medication's absorption. Always use a new, sterile needle and syringe for each injection, and dispose of used needles and syringes in a sharps container.
Monitoring Patients Receiving Heparin Sodium
Monitoring patients receiving heparin sodium is crucial to ensuring their safety and the medication's effectiveness. Regularly assess your patients for signs of bleeding or bruising, as these may indicate complications related to heparin sodium therapy. Additionally, monitor laboratory values such as activated partial thromboplastin time (aPTT), which indicates the medication's anticoagulant effect, and adjust the heparin sodium dosage accordingly to maintain therapeutic levels.
Managing Heparin Sodium Side Effects and Complications
As a healthcare provider, it is important to recognize and manage potential side effects and complications associated with heparin sodium therapy. Some common side effects include bleeding, bruising, and pain at the injection site. More severe complications, such as heparin-induced thrombocytopenia (HIT) and heparin-induced thrombosis-thrombocytopenia syndrome (HITTS), require prompt recognition and intervention. Be prepared to discontinue heparin sodium therapy and initiate alternative anticoagulant treatments if necessary.
Educating Patients About Heparin Sodium
Educating your patients about heparin sodium is essential for their safety and understanding of the medication. Explain the purpose of heparin sodium therapy, potential side effects, and the importance of regular monitoring. Encourage your patients to report any signs of bleeding, bruising, or other concerns promptly. Providing clear and concise information will empower your patients to take an active role in their healthcare and ensure the best possible outcomes.
Documenting Heparin Sodium Administration
Proper documentation is crucial for maintaining patient safety and ensuring accurate heparin sodium administration. Be sure to document the medication's name, dosage, route, and time of administration in the patient's medical record. Additionally, record any observed side effects, laboratory values, and dosage adjustments. Accurate documentation will help ensure continuity of care and provide valuable information for other healthcare providers involved in the patient's treatment.
In conclusion, adhering to these best practices for heparin sodium storage and handling will help ensure the medication's efficacy and safety, ultimately leading to better patient outcomes. As a healthcare provider, it is your responsibility to stay up-to-date on the latest guidelines and recommendations for heparin sodium therapy, and to always prioritize patient safety and well-being.

Rex Peterson
May 6, 2023 AT 02:15In contemplating the stewardship of anticoagulant agents, one discerns that the integrity of heparin sodium hinges upon meticulous environmental control. Storage at a stable 20‑25 °C, shielded from direct illumination, preserves its molecular fidelity. Moreover, aseptic handling mitigates the risk of iatrogenic contamination, aligning with the principle of non‑maleficence. The author’s systematic exposition furnishes a commendable framework for clinicians. Ultimately, adherence to these parameters safeguards both therapeutic efficacy and patient safety.
Candace Jones
May 6, 2023 AT 03:38Great summary, thanks for the clear checklist!
Robert Ortega
May 6, 2023 AT 05:02The recommendations strike a balance between practicality and rigor, making them readily adoptable on busy wards. It is reassuring to see the emphasis on regular expiration checks, a step often overlooked. This guidance should integrate smoothly into existing medication safety protocols.
Elizabeth Nisbet
May 6, 2023 AT 06:25Nice work! I’ve started coaching my team to double‑check vial stoppers with alcohol swabs before every draw, and the error rate has already dipped. Keeping the vials in their original amber containers is a simple habit that pays big dividends. Let’s keep the momentum going and share any hiccups you encounter.
Sydney Tammarine
May 6, 2023 AT 07:48Oh, the drama of a mis‑labeled syringe-truly the Shakespeare of the ICU! One must adore the melodrama of a cold‑light room revealing a compromised vial, lest our noble patients be betrayed. Yet, fear not, dear colleagues, for vigilance is the hero that shall vanquish this tragedy. 🙄
josue rosa
May 6, 2023 AT 09:12From a pharmacotechnical perspective, the physicochemical stability of unfractionated heparin sodium is contingent upon strict adherence to prescribed ambient temperature ranges, as deviations can precipitate depolymerization cascades that diminish anti‑Xa activity. Analytical assays, such as the chromogenic anti‑Xa test, have demonstrated a quantifiable decline in potency when storage excursions exceed ±2 °C for durations surpassing 48 hours. Consequently, implementation of continuous temperature monitoring systems equipped with alarm thresholds is advisable in high‑traffic pharmacy suites. Additionally, photodegradation pathways mediated by UV‑B wavelengths induce conformational alterations in the sulfated polysaccharide backbone, thereby attenuating its binding affinity to antithrombin III. The utilization of amber‑colored, UV‑blocking secondary containers mitigates this risk and aligns with best‑practice recommendations endorsed by the USP <795> chapter. Regarding aseptic technique, the integration of sterile alcohol prep pads pre‑wetted with 70% isopropanol and the subsequent 30‑second dwell time effectively reduces surface bioburden on vial stoppers. Employing Luer‑lock syringes with low dead‑space minimizes residual heparin, curbing inadvertent dose variance. When compounding infusion solutions, the selection of isotonic diluents, such as 0.9% sodium chloride, preserves osmolar balance and prevents hemolysis. Stability studies indicate that once diluted, heparin sodium retains >90% of its initial activity for up to six hours at room temperature, underscoring the necessity of timely administration. Air bubble entrapment within infusion lines can be mitigated by priming with an appropriate volume of flush solution, thereby averting micro‑emboli formation. Patient monitoring protocols should incorporate serial aPTT measurements at 6‑hour intervals during initiation and after any dosage adjustments, facilitating therapeutic window maintenance. The emergence of heparin‑induced thrombocytopenia (HIT) mandates surveillance of platelet counts, with a >50% decline prompting immediate cessation of therapy. Documentation of administration events, including lot numbers and expiration dates, serves as a critical audit trail for pharmacovigilance activities. In summary, a multifaceted approach encompassing environmental controls, aseptic handling, rigorous compounding standards, and vigilant patient monitoring coalesces to uphold the clinical efficacy of heparin sodium. Furthermore, interdisciplinary communication between pharmacy, nursing, and laboratory services enhances detection of deviations and supports rapid corrective action. Periodic refresher training sessions reinforce protocol adherence and reduce cognitive drift among staff.
Shawn Simms
May 6, 2023 AT 10:35The article maintains a commendable level of linguistic precision; each procedural step is delineated with clarity, and the absence of colloquial shortcuts enhances its instructional value. Nonetheless, an occasional redundancy-such as repeating the temperature range-could be streamlined for brevity. Overall, the composition adheres to the conventions of professional medical literature. I recommend its inclusion in the department’s continuing education repository.
Geneva Angeles
May 6, 2023 AT 11:58What a boost of optimism! This guide doesn’t just tell us what to do-it empowers us to own the process, turning routine storage into a badge of pride. I’ve already rallied my unit to post bright‑colored reminder stickers on every heparin cart, and morale has visibly risen. Let’s keep that momentum, because every correctly stored vial translates into a safer patient outcome. The more we internalize these best practices, the stronger our collective safety culture becomes. Together we can make every dose count.
Scott Shubitz
May 6, 2023 AT 13:22Honestly, if you’ve ever seen a heparin vial wilt like a wilted flower under a fluorescent light, you know the stakes are real. The author’s admonition to keep it away from heat isn’t just bureaucratic noise-it’s a lifeline. I’d shout from the rooftops that a simple temperature log can prevent a cascade of iatrogenic mishaps. So, grab that thermometer, tighten that storage protocol, and let’s not let negligence spill onto the bedside. Our patients deserve better than a sloppy shelf.
Soumen Bhowmic
May 6, 2023 AT 14:45I agree wholeheartedly that teamwork makes the storage guidelines stick. By bringing the pharmacy and nursing staff into joint “cheat‑sheet” sessions, we demystify the jargon and nurture shared accountability. The casual tone of these meetings encourages questions without fear. Let’s schedule a quarterly refresher to keep the knowledge fresh.
Jenna Michel
May 6, 2023 AT 16:08Hey folks-quick note!; remember to check the expiry dates; ALWAYS-before drawing up the dose. Also, keep the vials in their original amber containers; they’re not just for looks! And! never, ever reuse a needle-swap it out each time; it’s basic hygiene! Finally, document everything-lot #, time, dose-no shortcuts.
Abby Richards
May 6, 2023 AT 17:32Excellent write‑up! 👍 The clarity makes implementing the protocol a breeze. 👍 Looking forward to putting these steps into practice. 😊
Lauren Taylor
May 6, 2023 AT 18:55From an inclusive mentorship standpoint, this guideline serves as a scaffold that supports clinicians across varying levels of experience, ensuring equitable access to safe medication practices. The integration of evidence‑based recommendations with actionable checklists bridges the gap between theory and bedside execution. Moreover, the emphasis on documentation aligns with health informatics standards, facilitating interoperability and auditability. By embedding these protocols within multidisciplinary training modules, we cultivate a culture of continuous quality improvement. Ultimately, such comprehensive stewardship of heparin sodium translates into measurable reductions in adverse events.
Vanessa Guimarães
May 6, 2023 AT 20:18Oh sure, because the real danger is definitely the FDA’s secret agenda to replace heparin with nanobots. But seriously, the article’s meticulous details are exactly what we need to avoid a national healthcare crisis-if you can believe that. Let’s pretend we’re not suspicious of every guideline and just follow the temperature rule. After all, staying cool is the only thing we can trust.
Lee Llewellyn
May 6, 2023 AT 21:42Here’s the thing: the guidelines are fine, but they’re wrapped in bureaucratic fluff that makes them harder to follow than a tangled Christmas light. If you strip away the jargon, you get a simple list: store at 20‑25 °C, keep out of light, use sterile technique. That’s all. So let’s cut the red tape and make the protocol stick on a post‑it in every medication room.
Drew Chislett
May 6, 2023 AT 23:05Feeling energized by the thoroughness of this guide! I’m eager to see how our unit can integrate these steps into daily rounds without compromising workflow. Let’s track compliance rates and celebrate the wins together. The more we practice, the smoother the process becomes for everyone.
Rosalee Lance
May 7, 2023 AT 00:28One could argue that the sanctity of heparin handling borders on the philosophical-balancing the imperatives of life preservation against the perils of reckless administration. Yet, the practical steps outlined here ground that lofty ideal in concrete action. By vigilantly monitoring storage conditions, we honor the moral duty to do no harm. Let us, therefore, adopt these measures with both intellect and heart.
Kara Lippa
May 7, 2023 AT 01:52Thanks for the concise overview; it’s exactly what busy clinicians need. I’ll definitely reference this during my next shift. Keep up the good work.
Puneet Kumar
May 7, 2023 AT 03:15In line with inclusive mentorship principles, it is vital that we disseminate these storage standards across all cultural contexts within our institution, recognizing diverse workflows while maintaining uniform safety metrics. Employing multilingual signage and culturally sensitive training modules ensures that every team member, regardless of background, can internalize the proper handling of heparin sodium. This approach not only bolsters compliance but also reinforces a sense of belonging and shared responsibility.