TCA Therapeutic Range Calculator
Check Your TCA Blood Level
Enter your current blood level to see if it's within safe therapeutic ranges for tricyclic antidepressants
Enter your blood level to see results
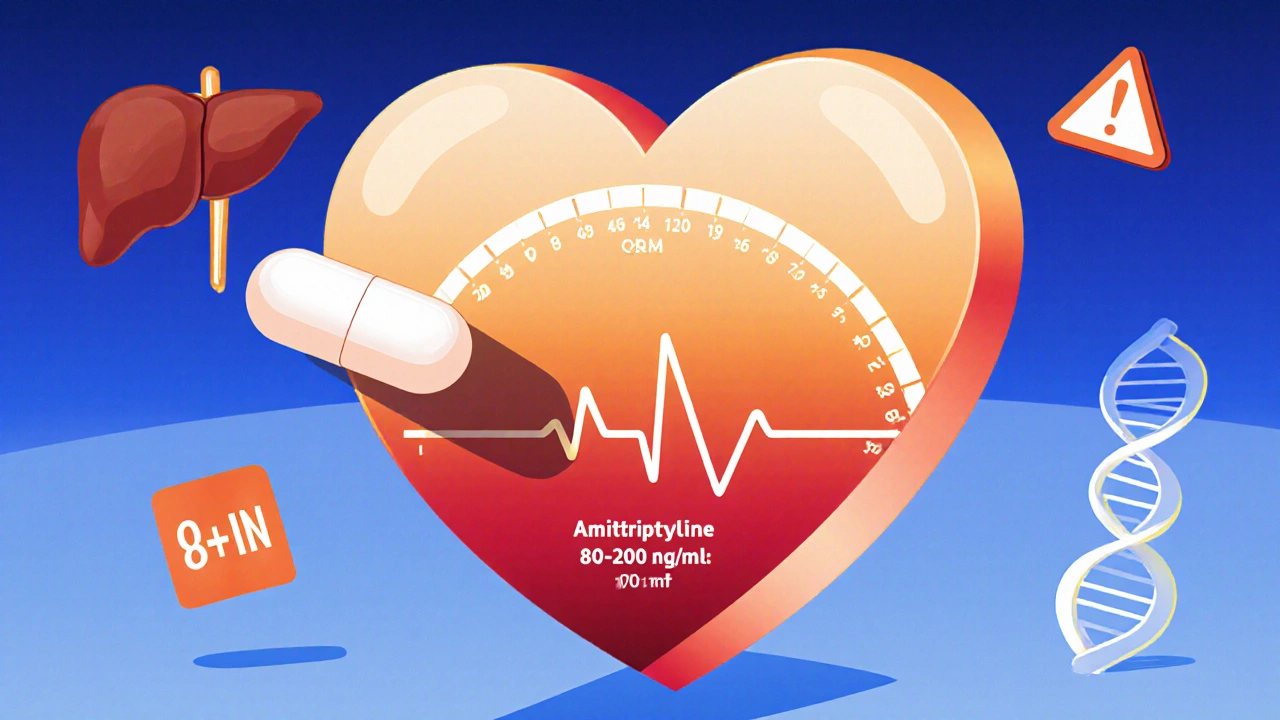
Tricyclic antidepressants (TCAs) like amitriptyline, nortriptyline, and desipramine were among the first effective treatments for depression. But they’re not safe for everyone. Even a small overdose - sometimes just one extra pill - can stop your heart. That’s why therapeutic drug monitoring isn’t optional for these drugs. It’s a lifeline.
Why TCAs Are Dangerous Even at Normal Doses
TCAs work by boosting serotonin and norepinephrine in the brain. That’s good for mood. But they also block a bunch of other receptors - in your heart, your gut, your eyes. This is why side effects like dry mouth, constipation, dizziness, and rapid heartbeat are so common. And when levels creep just a little too high, things turn deadly.
Here’s the hard truth: TCAs have one of the narrowest therapeutic windows of any psychiatric medication. For amitriptyline, the safe range is 80-200 ng/mL. Go above 500 ng/mL, and you’re in serious danger. At that level, your heart’s electrical system starts to misfire. Your QRS complex widens on an ECG - a sign your heart muscle can’t conduct signals properly. That can lead to ventricular arrhythmias, seizures, coma, or death.
And it doesn’t take much. A single tablet overdose has killed children. Older adults are especially vulnerable. Their livers slow down. Their kidneys don’t clear drugs as fast. A dose that’s fine for a 30-year-old can be lethal for a 70-year-old. That’s why TCAs are still used - but only with careful monitoring.
What Therapeutic Drug Monitoring Actually Does
Therapeutic drug monitoring (TDM) means measuring how much of the drug is in your blood. Not guessing. Not estimating. Measuring.
For TCAs, this isn’t about whether the drug is working. It’s about whether it’s killing you.
Doctors don’t just look at the dose you’re taking. They look at the actual concentration in your bloodstream. Why? Because two people can take the same pill - same dose, same weight, same age - and have wildly different blood levels. One might be at 120 ng/mL. The other at 400 ng/mL. The second person could be hours away from cardiac arrest.
TDM tells you that. It catches problems before you start having seizures or your heart goes haywire. Studies show that using TDM cuts hospitalization risk by 35% compared to just adjusting doses based on how someone feels.
The test is simple: a blood draw, usually right before your next dose (called a trough level). You need to be on the same dose for at least 5-7 days so your body reaches steady state. Then, labs use high-performance liquid chromatography (HPLC) or mass spectrometry to measure the exact amount. Results come back in 24-48 hours.
Therapeutic Ranges You Need to Know
Not all TCAs are the same. Each has its own safe zone.
- Amitriptyline: 80-200 ng/mL
- Nortriptyline: 50-150 ng/mL
- Desipramine: 100-300 ng/mL
These aren’t guesses. They’re based on decades of clinical data from thousands of patients. Levels below these ranges? You’re probably not getting relief. Above? You’re risking your life.
But here’s the catch: some labs use slightly different ranges. One lab might say 150 ng/mL is the max for nortriptyline. Another says 170. That’s why doctors need to know which lab did the test. And why they shouldn’t rely on TDM alone - they have to look at your symptoms too.
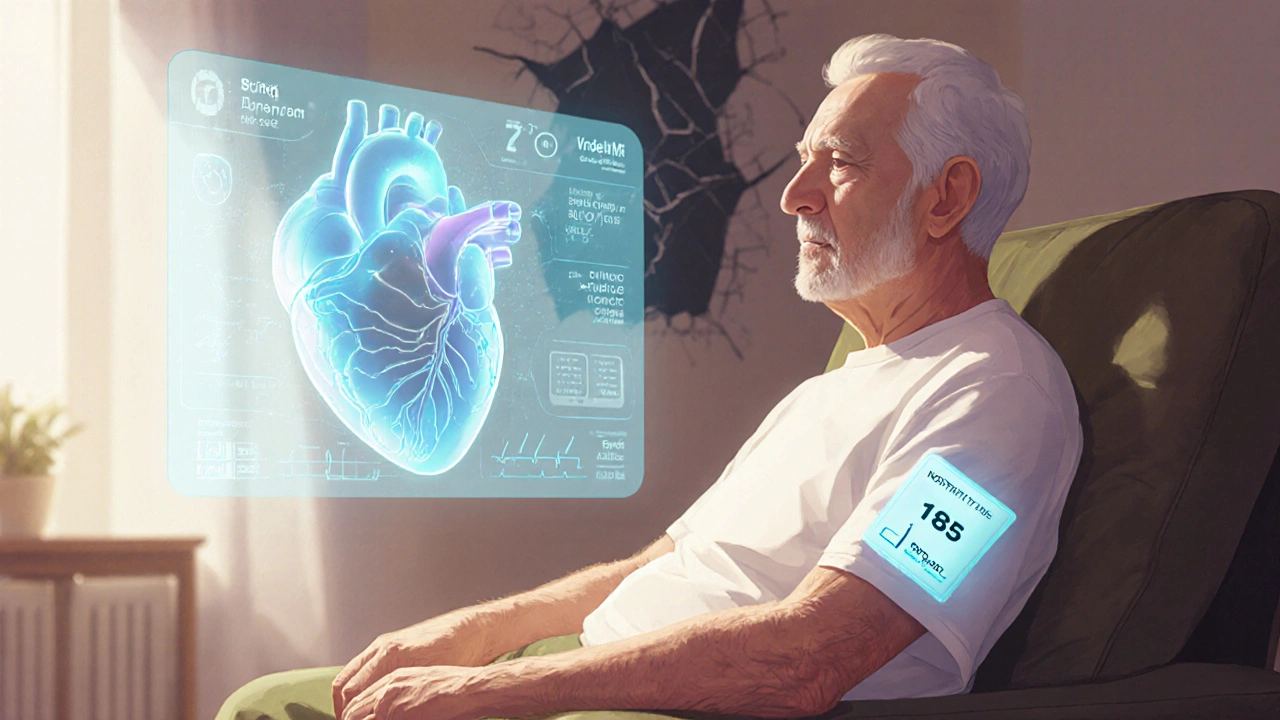
There was a case at Johns Hopkins where a 72-year-old man had nortriptyline levels at 185 ng/mL - way above the 150 ng/mL ceiling. He felt fine. No dizziness, no palpitations. But his ECG showed QRS widening. The team dropped his dose. He stayed out of the ICU. That’s TDM saving a life.
Why Some Patients Still Need TCAs
SSRIs like fluoxetine and sertraline are safer. That’s why they’re prescribed more often. But they don’t work for everyone.
For treatment-resistant depression - when nothing else helps - TCAs still work. For chronic nerve pain (like diabetic neuropathy or sciatica), nortriptyline is often the most effective option. In fact, 68% of pain specialists still start with it.
And for older adults with depression and insomnia? TCAs can help with both. Their sedating effect is a feature, not a bug. But that same sedation makes them dangerous if levels rise.
That’s why TCAs are still used - but only with TDM. It’s not about being outdated. It’s about using the right tool, safely.
The Hidden Risk: Drug Interactions and Genetics
One of the biggest reasons TDM fails isn’t bad testing. It’s bad information.
Many patients take other meds that mess with how TCAs are broken down. Common culprits: fluoxetine, paroxetine, bupropion, cimetidine, even some antibiotics. These drugs block the liver enzyme CYP2D6. If you’re on one of these and take a standard TCA dose, your blood level can spike - even if you haven’t changed your pill count.
And then there’s genetics. Some people are poor metabolizers. Their bodies process TCAs slowly. Others are ultrarapid metabolizers. They clear the drug too fast. The difference? Up to 30-fold in blood concentration. Two people. Same dose. One is fine. The other is in cardiac arrest.
That’s why more clinics are combining TDM with pharmacogenetic testing. If you know you’re a poor CYP2D6 metabolizer, you start with a quarter of the usual dose. No trial and error. No near-death experiences.
As of 2023, about one-third of U.S. academic medical centers now offer this combo. Mayo Clinic reported a 40% faster time to stable dosing when they did.
What Goes Wrong in Real Life
Even with all the science, mistakes happen.
A 2017 study across 12 European hospitals found that 37.5% of TDM requests didn’t list what other drugs the patient was taking. 28% of blood draws happened too early - before steady state. That means doctors were making decisions based on false data.
And 20% of dosage changes were wrong because someone misread the report. A level of 190 ng/mL? Looks fine - until you realize it’s for amitriptyline, and the max is 200. But the patient has heart disease. And they’re 78. That level might be too high anyway.
One tragic case in Clinical Toxicology involved a 42-year-old woman with amitriptyline at 190 ng/mL - technically within range. But her QRS was 140 ms. She had a seizure. She survived. But she shouldn’t have been anywhere near that level.
That’s the lesson: numbers alone aren’t enough. You need the ECG. You need the symptoms. You need the full picture.
What’s New in TDM
Technology is catching up.
Siemens Healthineers just launched a handheld TCA monitor in Europe. It gives results in 20 minutes - not two days. Sensitivity? 5 ng/mL. That’s precise enough to catch early toxicity.
The FDA cleared an AI platform called PsychX Analytics that links your TCA level to your ECG, age, and other meds. It predicts your risk of toxicity before you even feel sick. It’s not perfect - but it’s a big step.
Researchers at the National Institute of Mental Health are testing a patch that measures TCA levels in interstitial fluid. Early results show 92% correlation with blood tests. No needles. Just a sticker on your arm.
And soon, doctors may use genetic data to set your first dose - so you never have to go through dangerous highs and lows.
When TDM Isn’t Enough
If someone overdoses - whether by accident or intent - you don’t wait for a blood test.
Emergency treatment is immediate: sodium bicarbonate to correct heart rhythm, activated charcoal if it’s been less than two hours, and intensive monitoring. The ECG is your first alarm. QRS >100 ms? Treat it like a cardiac emergency - even if the drug level is “normal.”
TDM is for prevention. Not rescue.
Who Should Get TDM for TCAs?
Not everyone. But these people definitely should:
- Patients over 60
- Those with heart disease or history of arrhythmias
- People taking other drugs that affect CYP2D6 or CYP2C19
- Those who haven’t improved after 2-4 weeks
- Anyone with side effects like dizziness, confusion, or rapid heartbeat
- Patients with kidney or liver disease
For young, healthy adults with no other meds and no risk factors? TDM might not be needed. But for the rest? It’s non-negotiable.
Final Takeaway: TDM Isn’t Optional - It’s Essential
TCAs are powerful. They can lift depression. They can ease pain. But they can also kill.
Therapeutic drug monitoring turns guesswork into science. It’s the difference between hoping a dose is safe and knowing it is.
The American Psychiatric Association says TDM for TCAs is a Level 1 recommendation - the highest level of evidence. That means: do it.
If you’re on a TCA, ask your doctor: “Have you checked my blood level?” If they haven’t, push for it. If they say, “You’re feeling fine, so it’s not needed,” ask why. Because feeling fine doesn’t mean your heart is safe.
One pill too many. One lab error. One missed interaction. That’s all it takes.
Don’t let it be you.
What is therapeutic drug monitoring (TDM) for tricyclic antidepressants?
Therapeutic drug monitoring (TDM) for tricyclic antidepressants (TCAs) is the process of measuring the concentration of the drug in your bloodstream to ensure it’s within a safe and effective range. Since TCAs have a narrow therapeutic window - meaning the difference between a helpful dose and a toxic one is small - TDM helps prevent life-threatening side effects like heart rhythm problems, seizures, or coma. Blood samples are taken at trough levels (just before your next dose) after 5-7 days of consistent use, and results guide dose adjustments.
What are the safe blood levels for common TCAs?
Safe blood levels vary by drug: amitriptyline (80-200 ng/mL), nortriptyline (50-150 ng/mL), and desipramine (100-300 ng/mL). Levels above 500 ng/mL are considered toxic and can cause severe cardiac and neurological effects. It’s important to note that these ranges are based on population data - individual sensitivity varies, so clinical symptoms and ECG changes must always be considered alongside blood levels.
Why are TCAs still used if they’re so dangerous?
TCAs are still used because they work when other antidepressants don’t - especially for treatment-resistant depression and chronic nerve pain. Nortriptyline, for example, is a first-line choice for neuropathic pain in 68% of pain specialists. They’re also effective for elderly patients with depression and insomnia. But because of their high toxicity risk, they’re only prescribed with strict monitoring, including TDM and ECG checks.
Can drug interactions affect TCA levels?
Yes. Many common medications - like fluoxetine, paroxetine, bupropion, cimetidine, and some antibiotics - block the liver enzyme CYP2D6, which breaks down TCAs. This can cause TCA levels to rise dangerously, even if your dose hasn’t changed. That’s why it’s critical to tell your doctor every medication, supplement, or herb you’re taking before starting a TCA.
Is genetic testing helpful with TCA monitoring?
Yes. Genetic testing for CYP2D6 and CYP2C19 enzymes can reveal whether you’re a poor, normal, or ultrarapid metabolizer. Poor metabolizers may need a quarter of the standard dose, while ultrarapid metabolizers might need more. Combining genetic testing with TDM reduces the time to find the right dose by up to 40% and prevents dangerous fluctuations in blood levels.
How often should TDM be done for TCAs?
TDM is typically done after 5-7 days of stable dosing to reach steady state. After that, it’s repeated if the dose changes, if side effects appear, if new medications are added, or if the patient is elderly or has liver/kidney problems. Some patients need testing every few months. Others may only need it once, if they respond well and stay stable.
What should I do if I miss a blood draw for TDM?
If you miss a scheduled blood draw, reschedule it as soon as possible - but don’t skip it. If you’re feeling fine, don’t assume your levels are safe. TCAs can build up silently. If you’re due for a test and can’t get to the lab, talk to your doctor. They may delay a dose increase or recommend an ECG in the meantime. Never adjust your dose without knowing your blood level.
Can TDM prevent TCA overdose deaths?
Yes. Studies show TDM reduces hospitalization risk by 35% and adverse events by 25-30% when used properly. It catches toxicity before symptoms appear - like QRS widening on an ECG - allowing doctors to lower doses before cardiac arrest happens. In real-world cases, TDM has prevented ICU admissions and saved lives, especially in elderly patients who are more vulnerable to even small changes in drug levels.

Ellen Calnan
November 18, 2025 AT 23:01This post hit me like a freight train. I’ve been on nortriptyline for five years, and no one ever checked my levels until I had a near-miss with ventricular tachycardia. They just said, 'You seem fine.' Fine doesn’t mean your heart isn’t screaming. I’m alive because I demanded a blood test after reading a forum post about QRS widening. Don’t wait for a seizure to ask questions.
Richard Risemberg
November 20, 2025 AT 02:15Let’s be real-TCAs are the dark horses of psychiatry. Sleek, powerful, but one wrong gear shift and you’re off the cliff. I’ve seen patients on 25mg of amitriptyline crash because they started taking an OTC cold med with diphenhydramine. No one tells you that. Pharmacists don’t always know. Doctors assume you’re not mixing stuff. Spoiler: you are. TDM isn’t just good practice-it’s the only thing standing between someone and an obituary written in ECG lines.
Andrew Baggley
November 20, 2025 AT 14:11If your doctor isn’t ordering TDM for TCAs, fire them. Seriously. This isn’t debate territory. It’s basic safety. I’m a nurse in an ER that sees three TCA overdoses a month. Half of them were ‘just taking their meds as prescribed.’ One guy was on 75mg of desipramine-‘normal’ dose-because his CYP2D6 is broken. Genetic testing would’ve saved him six weeks of agony. Stop guessing. Start testing.
Frank Dahlmeyer
November 21, 2025 AT 14:35Let me tell you about the time I was managing a 76-year-old woman on amitriptyline for depression and neuropathic pain. She was doing great-until she started taking cimetidine for heartburn. No one connected the dots. Her TCA level spiked to 480 ng/mL. She didn’t feel different. No dizziness. No nausea. Just a quiet, creeping QRS widening on her ECG. We caught it because her daughter insisted on a blood test after reading this exact article. She’s alive today because someone refused to accept ‘you’re fine’ as an answer. TDM isn’t bureaucracy-it’s the last line of defense for people who can’t scream loud enough. And if your clinic doesn’t offer it, push until they do. Lives are not optional.
Codie Wagers
November 22, 2025 AT 00:22There is a profound moral failure in psychiatry when we allow patients to be dosed empirically with drugs that have a therapeutic window narrower than lithium. The fact that TDM is not universally mandated for TCAs is not negligence-it is institutionalized malpractice. You cannot justify a 35% reduction in hospitalization rates with ‘we’ve always done it this way.’ This isn’t medicine. It’s Russian roulette with a tricyclic bullet. The APA’s Level 1 recommendation should be federal law. And anyone who says ‘she’s feeling fine’ should be required to sit through a 12-hour cardiac arrest simulation. Just once.
Reema Al-Zaheri
November 23, 2025 AT 21:10harenee hanapi
November 24, 2025 AT 05:23Everyone’s acting like this is new news. I’ve been screaming about this since 2018. My cousin died from a TCA overdose. They told her mom, 'She was just taking her pills.' She was. And her levels were 620 ng/mL. The lab report got lost. The doctor didn’t follow up. She was 54. No heart disease. No other meds. Just… unlucky. Now everyone’s shocked? Wake up. This happens every week. And no one’s doing anything. I’m tired of being the only one who remembers.
Christopher Robinson
November 25, 2025 AT 20:45Just had my first TDM done last month after 3 years on nortriptyline. Level was 162 ng/mL-way above the 150 ceiling. Felt fine. ECG was fine. But my doc dropped my dose anyway. Said, 'Better safe than sorry.' 🙏 I’m not mad. I’m grateful. This is what medicine should look like: data + care. Not guesswork. Not ego. Just science that doesn’t wait for a heart to stop before acting. If you’re on a TCA, ask for the test. It’s not a sign you’re broken-it’s a sign you’re smart. 💉🧠