Low blood sugar isn’t just a nuisance-it can be dangerous. If you’re taking insulin, sulfonylureas, or meglitinides for diabetes, you’re at real risk for hypoglycemia. Blood glucose below 70 mg/dL triggers symptoms like shaking, sweating, and confusion. Below 54 mg/dL, you could pass out or have a seizure. This isn’t theoretical. One in four people with type 1 diabetes after 20 years loses the ability to feel these warning signs. And it’s not just about insulin-some oral meds carry the same risk. The good news? You can manage it. Not by avoiding your meds, but by understanding them, planning ahead, and using the right tools.
Know Which Medications Put You at Risk
Not all diabetes drugs cause low blood sugar. Metformin? Almost zero risk. GLP-1 agonists like semaglutide? Less than 2%. SGLT2 inhibitors like empagliflozin? Around 3%. But if you’re on insulin, sulfonylureas (glimepiride, glipizide, glyburide), or meglitinides (repaglinide, nateglinide), your risk jumps to 15-40% per year. Sulfonylureas are especially tricky-they keep pushing insulin out even when your blood sugar drops. That’s why many doctors now avoid them in older adults or those with kidney issues. If you’re on one of these meds and you’ve had a low blood sugar episode, talk to your provider. There are safer alternatives.Recognize the Signs-Before It’s Too Late
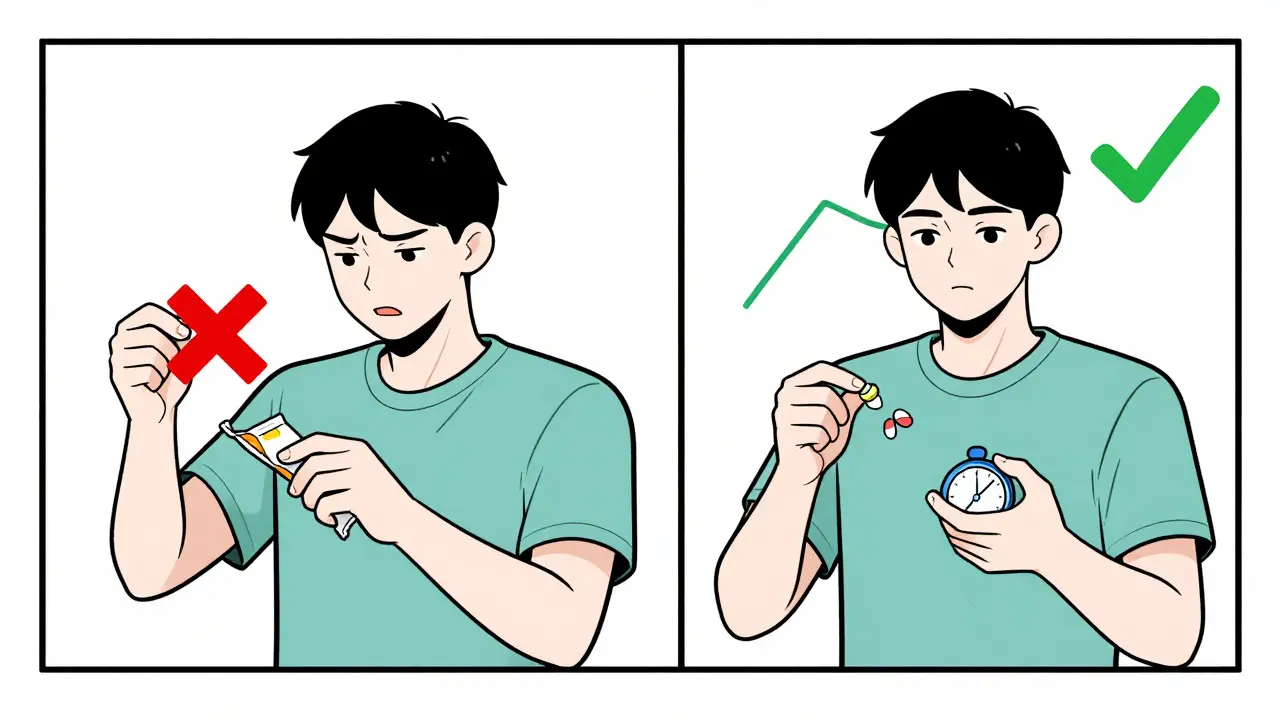
Hypoglycemia hits in two waves. First, your body sends out alarms: heart racing, sweating, trembling, hunger. These happen around 65-70 mg/dL. If you ignore them, your brain starts to starve. That’s when things get serious-confusion, slurred speech, drowsiness, seizures. This happens below 55 mg/dL. The scary part? After years of diabetes, especially type 1, your body stops sending those early warnings. That’s called hypoglycemia unawareness. It affects 25% of long-term type 1 patients and 10% of type 2 patients after 15 years. If you’ve had a low without warning, you’re in the high-risk group. You need a different plan.Follow the 15-15 Rule-Exactly
When your blood sugar drops below 70 mg/dL, act fast. Not with candy bars, not with juice boxes, not with sugar-free snacks. Use 15 grams of fast-acting glucose. That’s:- 3-4 glucose tablets (like Glucola or Glukos)
- 4 ounces of regular soda (not diet)
- 1 tablespoon of honey or sugar
- Half a cup of fruit juice
Carry Emergency Gear-Always
If you’re at risk for severe lows, you need glucagon. Not just in case you pass out-because someone else might need to help you. Traditional glucagon kits require mixing powder and liquid. That takes 3 minutes. You won’t have that time if you’re unconscious. Newer options change everything:- Baqsimi: Nasal spray. One puff. No mixing. $250.
- Gvoke: Prefilled syringe. Just inject. $350.
- Zegalogue: Liquid glucagon. Ready in 10 seconds. FDA-approved in 2023.
Use Continuous Glucose Monitoring (CGM)
A fingerstick test tells you your blood sugar at one moment. A CGM shows you the whole story-trends, spikes, drops, and overnight lows you never knew about. Studies show CGMs reduce hypoglycemia time by 35% and severe events by 48%. The Dexcom G7 and Freestyle Libre 3 are now small, painless, and accurate. But cost is a barrier. Medicare covers CGMs for insulin users, but out-of-pocket costs still hit $89 to $399 per month. If you’re struggling to afford one, ask your provider about patient assistance programs. Many manufacturers offer copay cards or free trials. And if you’re on insulin, you’re likely eligible under new Medicare rules. Don’t assume you can’t get it-ask.Track Patterns, Not Just Numbers
HbA1c doesn’t tell you the whole story. Someone can have an HbA1c of 7% and still have dangerous lows hiding in the data. That’s why logging matters. Use a simple logbook: record your meds, meals, activity, and glucose readings. The Joslin Diabetes Center found patients who did this daily reduced hypoglycemia by 52% in six months. Look for patterns. Do you always go low after afternoon walks? After skipping lunch? After drinking alcohol? Alcohol causes 22% of severe lows in people under 40. Exercise without carb adjustment causes 31% of daytime lows. If you notice a trend, adjust. Maybe take a snack before your walk. Maybe reduce your insulin dose on workout days. Don’t guess. Track.Adjust for Life-Not Just Diabetes
Your meds don’t live in a vacuum. Alcohol, exercise, stress, illness, sleep-all change how your body responds. If you’re going out for drinks, eat something first. Don’t drink on an empty stomach. If you’re exercising, check your glucose before, during, and after. You may need to lower your insulin dose or eat extra carbs. If you’re sick, your body might need less insulin-but you might also skip meals. That’s a recipe for low blood sugar. Talk to your provider about sick-day rules. And if you’re on beta-blockers for high blood pressure, you might not feel the warning signs. That’s a hidden risk. Your doctor needs to know.
Get Trained-It Makes a Difference
Most people learn how to handle low blood sugar by trial and error. That’s dangerous. The ADA’s “Hypoglycemia Uncovered” program shows that patients who get 60 minutes of structured training reduce low blood sugar episodes by 45% in six months. Training includes:- How to read your CGM trends
- How to count carbs accurately (not estimate)
- When and how to use glucagon
- How to adjust meds for activity or meals
Know When to Call for Help
If you’re confused, can’t swallow, or pass out-call 911. Don’t wait. Don’t try to give someone food or juice if they’re unconscious. That can choke them. Use glucagon if you have it. If not, call for help. Emergency rooms see over 10% of diabetes hospitalizations because of severe hypoglycemia. That’s $4.1 billion a year in costs. But most of these are preventable. If you’ve had two or more severe lows in a year, talk to your doctor. Your treatment plan needs a reset.What’s Next? The Future Is Here
Closed-loop insulin systems-like the Tandem x2 with Control-IQ-are already cutting nighttime lows by 3.1 hours per night. AI-driven dosing algorithms are being tested to reduce hypoglycemia by 60%. These aren’t sci-fi. They’re available now. And by 2030, 75% of insulin users will likely use them. You don’t have to wait for the future. Start with what’s possible today: a CGM, glucagon, a logbook, and a plan. You’re not stuck with the risks of your meds. You have tools. You have knowledge. You just need to use them.Can metformin cause low blood sugar?
No, metformin alone does not cause hypoglycemia. It works by reducing liver glucose production and improving insulin sensitivity, not by forcing insulin release. The risk is less than 5% when used by itself. However, if you take metformin with insulin, sulfonylureas, or meglitinides, your risk increases because of the combined effect. Always check with your doctor before changing combinations.
Why do I get low blood sugar at night?
Nighttime lows often happen because your long-acting insulin peaks while you sleep, or your evening meal didn’t have enough carbs. Alcohol, exercise earlier in the day, or skipping dinner can also trigger them. CGMs are the best tool to catch these-many will alarm if your glucose drops while you’re asleep. Set your alert to 70 mg/dL and consider a small bedtime snack with protein and complex carbs if you’re prone to overnight lows.
Should I stop my diabetes medication if I keep getting low?
Never stop your medication without talking to your doctor. Stopping insulin or sulfonylureas suddenly can cause dangerously high blood sugar. Instead, review your logbook with your provider. You may need a lower dose, a different timing, or a switch to a safer drug. Many people can reduce or eliminate lows by adjusting their plan-not by quitting meds.
Are glucose tablets better than juice for treating low blood sugar?
Yes, glucose tablets are better. They’re pure glucose, absorbed quickly and predictably. Juice can vary in sugar content-some have added water or flavoring. Plus, juice often contains calories you don’t need. Glucose tablets are portioned at 15 grams per serving, so you know exactly what you’re taking. They’re also easier to carry and don’t spill. Keep them in every bag you own.
Can I use a smartwatch to monitor my blood sugar?
No. Smartwatches can track heart rate, sleep, and steps-but none currently measure blood glucose accurately. Only FDA-cleared CGMs like Dexcom, Freestyle Libre, or Medtronic systems can do that. Some watches can display CGM data, but they don’t replace the sensor. Don’t rely on a watch alone. Use a proper CGM if you’re at risk for lows.
How often should I check my blood sugar if I’m on insulin?
At least 4 times a day-before meals and at bedtime. If you’re using a CGM, you’re getting continuous data, so you can check less often. But still test with a fingerstick if your CGM reads low, if you feel symptoms, or if you’re sick. If you’ve had a recent low, check more often for the next 24 hours. Consistency saves lives.


SHAKTI BHARDWAJ
December 25, 2025 AT 22:08so i tried the 15-15 rule and it worked once... then i ate a whole bag of skittles because my brain was like NOPE and now i’m in the hospital again lol
Matthew Ingersoll
December 26, 2025 AT 01:15Glucagon is non-negotiable. I carry two. One in my coat, one in my car. If you’re on insulin and don’t have it, you’re playing Russian roulette with your brain.
Alex Ragen
December 27, 2025 AT 23:15One must interrogate the epistemological foundations of hypoglycemic awareness: Is the body’s ‘alarm system’ truly a biological signal-or merely a conditioned response to chronic metabolic dysregulation? The loss of warning symptoms, as the author notes, is not a failure of physiology, but a surrender of homeostatic autonomy to pharmacological intervention. We are, in essence, outsourcing our autonomic nervous system to pharmaceutical corporations-and then marveling when it malfunctions.
And yet, the 15-15 Rule, while statistically efficacious, remains a crude, reductionist intervention-reducing a complex neuroendocrine crisis to a sugar tablet. One wonders whether we are treating the symptom, or merely distracting the body from its own wisdom.
Lori Anne Franklin
December 28, 2025 AT 21:38Just wanted to say thank you for this post-seriously. I’ve been on insulin for 12 years and never knew about Baqsimi until now. I just ordered one. Also, I spell glucose wrong like 80% of the time but I’m learning 😅
Dan Alatepe
December 29, 2025 AT 17:36Man, I used to think my night lows were just ‘bad luck’-turns out I was drinking beer after gym without eating. Now I keep peanut butter packets in my gym bag. Life changed. Nigeria ain’t got CGMs easy, but I beg, borrow, and steal to keep mine charged.
Angela Spagnolo
December 30, 2025 AT 23:53I’ve been using a CGM for 18 months... and I still get startled when it beeps at 3 a.m. But I’ve had zero severe lows since. It’s not perfect, but it’s my guardian angel. Also, I think everyone should read this twice. And then read it again.
Sarah Holmes
January 1, 2026 AT 20:41It’s deeply irresponsible that pharmaceutical companies market sulfonylureas as ‘first-line’ for elderly patients while knowing full well the risk profile. This isn’t medical advice-it’s a death sentence disguised as a prescription. The FDA should be ashamed.
Jay Ara
January 2, 2026 AT 20:08you got this. i used to panic every time my sugar dropped, now i just grab my glucose tabs and breathe. small steps. you’re not alone.
Michael Bond
January 3, 2026 AT 12:30CGM > fingersticks. Period.
Kuldipsinh Rathod
January 5, 2026 AT 06:06i used to think juice was fine till i saw how long it took my sugar to come up. now i only use tabs. also, my dog knows when i’m low-he licks my hand. weird but true.
carissa projo
January 6, 2026 AT 05:22I used to think hypoglycemia was just something that happened to ‘other people’-until I passed out at my daughter’s soccer game. I didn’t even feel it coming. That’s when I started tracking everything. Now I have a little notebook with my name on it. I don’t just manage diabetes-I manage my life. And I’m still here. You can be too.
It’s not about perfection. It’s about showing up. Even on the days you forget your tabs. Even when the CGM glitches. Even when you’re tired. You’re still fighting. And that matters.
Don’t wait for a crisis to get trained. Don’t wait for someone else to tell you it’s okay to ask for help. You deserve to live without fear. And you’re not alone in this.
josue robert figueroa salazar
January 6, 2026 AT 06:37glucose tablets are just sugar with a fancy name. same as juice. stop pretending it’s science.
david jackson
January 7, 2026 AT 18:10Okay, so let me get this straight-your body’s natural defense system against low blood sugar shuts down after 20 years of diabetes, so you’re supposed to replace it with a nasal spray that costs $250 and a $400/month CGM? And if you can’t afford it, you’re just supposed to… hope? That’s not a plan. That’s a privilege. This article reads like a luxury catalog for people who have insurance and a trust fund. What about the rest of us? The ones who choose between insulin and groceries? The ones who work two jobs and can’t afford to ‘track patterns’? This isn’t empowerment. It’s a guilt trip wrapped in medical jargon.
I’ve had three severe lows in three years. I don’t have glucagon. I don’t have a CGM. I have a phone, a juice box, and a prayer. And you know what? I’m still alive. Maybe the real problem isn’t the meds-it’s the system that makes survival optional.
Jody Kennedy
January 9, 2026 AT 01:39Just got my first CGM last week and I’m obsessed. I saw a drop at 2 a.m. I ate a banana and went back to sleep. No panic. No chaos. It’s like having a personal bodyguard. Also, I now know why I’m always tired after lunch. Spoiler: I’m crashing. Thanks for the wake-up call, literally.
christian ebongue
January 9, 2026 AT 23:10glucagon? yeah, i have it. also have a note on my fridge: ‘if i’m unconscious, don’t feed me. just spray or jab.’ my wife says i’m dramatic. i say i’m prepared.