When You Stop Breathing at Night, Your Heart Pays the Price
If you snore loudly, wake up gasping, or feel exhausted even after a full night’s sleep, you might have sleep apnea. It’s not just a nuisance - it’s a silent threat to your heart. About 1 billion people worldwide have sleep apnea, and in the U.S. alone, 40 million adults are affected. Most of these cases - 80 to 90% - are obstructive sleep apnea (OSA), where your throat muscles relax so much during sleep that your airway collapses. What happens next isn’t just about poor sleep. It’s about your heart struggling to survive each night.
Every time your breathing stops, your body goes into survival mode. Oxygen drops. Carbon dioxide builds up. Your brain jolts you awake - just enough to restart breathing, but not enough for real rest. These episodes can happen 5, 15, even 50 times an hour. And each one triggers a chain reaction that damages your cardiovascular system over time.
Why Your Blood Pressure Spikes When You Sleep
High blood pressure doesn’t just happen during the day. For people with sleep apnea, it often spikes at night - and never fully drops. Normally, your blood pressure falls by 10% or more while you sleep. This is called "dipping." But in 70 to 80% of people with moderate to severe sleep apnea, that dip never happens. Instead, their blood pressure stays high or even rises at night - a pattern called "non-dipping" or "reverse-dipping."
This isn’t random. Each time your airway closes, your body releases stress hormones like adrenaline. Studies show these hormone levels spike 2 to 4 times higher during apnea episodes than in normal sleep. That surge forces your blood vessels to tighten, making your heart work harder. Over months and years, this constant pressure turns into chronic hypertension.
Here’s the kicker: up to 80% of people with "resistant hypertension" - high blood pressure that won’t budge even after taking three different medications - also have undiagnosed sleep apnea. And if you’re under 40 and have high blood pressure, your odds of having sleep apnea are even higher. A 2024 study found young adults (20-40) with sleep apnea were 45% more likely to have hypertension than their peers without it. In older adults, the link is still there, but not nearly as strong.
How Sleep Apnea Leads to Heart Attacks and Strokes
It’s not just high blood pressure. Sleep apnea is a direct driver of heart attacks, strokes, and sudden cardiac death. People with moderate to severe sleep apnea have a 30% higher risk of developing coronary artery disease. Their risk of a fatal heart attack jumps by 60%. And the timing? It’s not random. A 2024 study of nearly 10,000 adults found that 26.5% of heart attacks in people with sleep apnea happened between midnight and 6 a.m. - compared to just 16.5% in people without it.
Why then? Because your heart is under maximum stress during those hours. Your blood pressure is already naturally higher in the early morning. Add in repeated oxygen drops, surging stress hormones, and the mechanical strain of fighting to breathe, and you’ve created the perfect storm for a clot or rupture in a narrowed artery.
Stroke risk is even more alarming. Sleep apnea more than doubles your chance of having a first stroke - and triples your risk of having another one. The worse your nighttime oxygen levels drop (below 90% for more than 12% of your sleep time), the higher your chance of dying from a stroke. One study found a 4.3 times higher stroke death rate in those with severe oxygen drops.

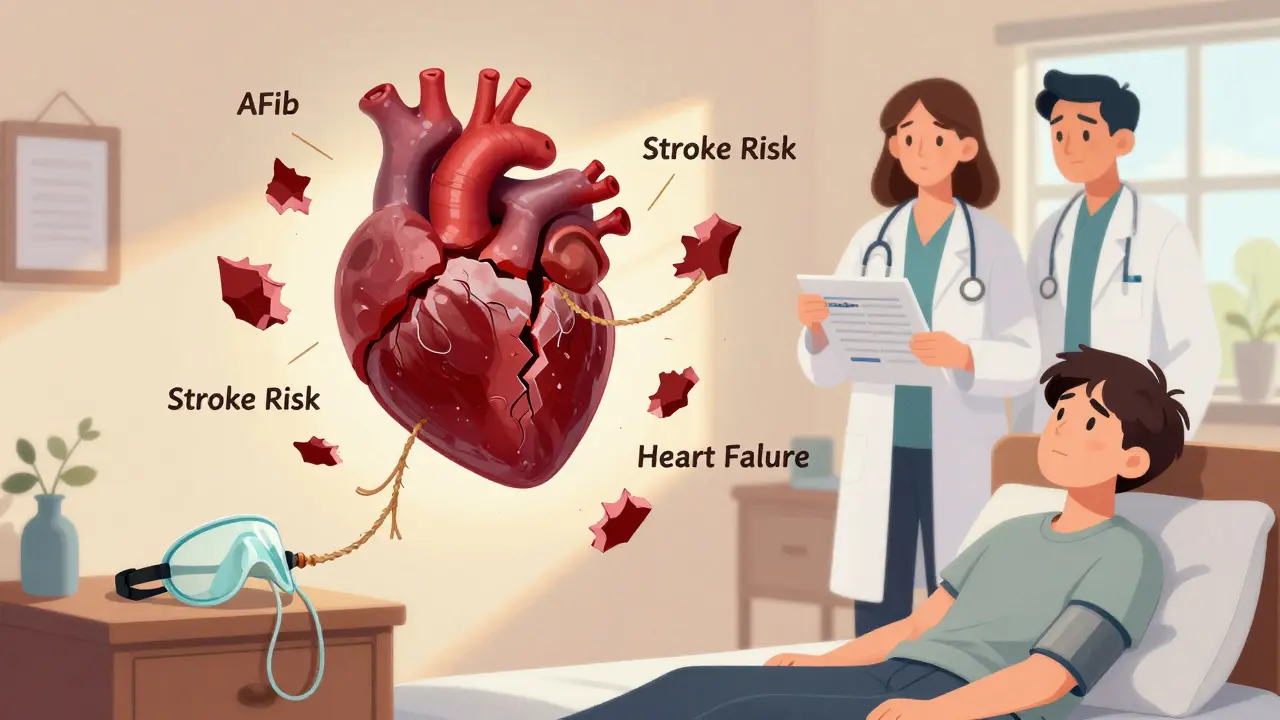
The Hidden Link Between Sleep Apnea and Heart Failure
Heart failure and sleep apnea don’t just coexist - they feed each other. About half of all heart failure patients also have sleep apnea. And for those without it, having sleep apnea increases your risk of developing heart failure by 140%.
Here’s how it works: when your airway collapses, your chest creates a powerful vacuum as you struggle to breathe. That pulls extra fluid into your heart and lungs, forcing your heart to pump harder. Over time, this strain weakens the heart muscle. At the same time, the repeated drops in oxygen trigger inflammation and scarring in heart tissue. The result? A heart that can’t pump efficiently.
There’s another layer: central sleep apnea, where the brain fails to send the right signals to breathe, is common in advanced heart failure. It’s a sign the heart is failing to regulate basic bodily functions. Treating it can improve survival - but only if it’s caught.
Arrhythmias: When Your Heart Goes Off-Rhythm
One of the most dangerous consequences of sleep apnea is irregular heartbeats - especially atrial fibrillation (AFib). People with sleep apnea are 2 to 4 times more likely to develop AFib. In one study, nearly half of patients with paroxysmal AFib (episodes that come and go) had undiagnosed sleep apnea, compared to just 21% of those without AFib.
And here’s what cardiologists see in practice: if you have AFib and untreated sleep apnea, your chances of success with catheter ablation - a common procedure to fix the rhythm - drop by 30%. The same goes for cardiac resynchronization therapy. Your heart device might work perfectly, but if your sleep apnea is still active, your body keeps sending the wrong signals, and your treatment fails.
Why Most People With Sleep Apnea Don’t Get Treated
Despite all this, 80% of people with moderate to severe sleep apnea have never been diagnosed. Why? Because symptoms are subtle. You might not remember waking up. You might just think you’re "always tired." Snoring is often dismissed as normal. And home sleep tests - while good at catching severe cases - miss up to 40% of mild sleep apnea.
Even when diagnosed, treatment is hard. Continuous positive airway pressure (CPAP) is the gold standard. It uses a mask to keep your airway open. But only 46% of users stick with it long-term. Most people quit because the mask is uncomfortable, the machine is noisy, or they don’t feel better right away.
And here’s the hard truth: CPAP doesn’t always lower blood pressure dramatically. Studies show it typically reduces systolic pressure by just 2-3 mmHg. But that’s not the whole story. CPAP cuts stroke recurrence by 37%. It improves heart failure outcomes. It makes AFib treatments work better. The benefits aren’t always in the numbers - they’re in preventing disasters.
What You Should Do If You’re at Risk
If you have high blood pressure, heart disease, AFib, or a history of stroke - and you snore, feel tired during the day, or wake up choking - get tested. The American Heart Association now says sleep apnea screening should be routine in these patients.
Ask your doctor about the STOP-Bang questionnaire. It’s simple: Do you Snore? Tired during the day? Observed stopping breathing? High blood Pressure? BMI over 35? Age over 50? Neck over 16 inches? Male? Answer yes to 3 or more, and your chance of moderate-to-severe sleep apnea is over 80%.
If you’re under 40 and have unexplained high blood pressure or early heart disease, don’t wait. Sleep apnea may be accelerating your risk. Early treatment can stop the damage before it’s permanent.
What’s Next? Better Screening, Better Care
The future isn’t just better machines - it’s better teamwork. Cardiologists, pulmonologists, and sleep specialists need to talk to each other. Patients shouldn’t have to jump between departments to get the care they need.
There’s also new research into personalized treatment. For some, weight loss can eliminate sleep apnea. For others, oral appliances or nerve stimulators might work better than CPAP. And for those with heart failure and central sleep apnea, new devices are being tested to restore normal breathing patterns.
The message is clear: sleep apnea isn’t a sleep problem. It’s a cardiovascular emergency. If your heart is struggling, your breathing might be the cause - and fixing it could save your life.