Brand-name drugs can cost hundreds-even over a thousand-dollars a month. If you’re insured but still struggling to pay for your medication, you’re not alone. Millions of Americans rely on manufacturer savings programs to make their prescriptions affordable. These aren’t scams or gimmicks. They’re real, legal discounts offered directly by drug companies. But using them correctly matters. Get it wrong, and you could end up paying more later-or worse, lose your discount overnight.
What Are Manufacturer Savings Programs?
Manufacturer savings programs are financial help tools created by pharmaceutical companies to lower what you pay at the pharmacy for brand-name drugs. The two main types are copay cards (or coupons) and patient assistance programs (PAPs). Copay cards cut your out-of-pocket cost per prescription-sometimes by 85% or more. PAPs are usually for people with very low income and may give you free medication.
These programs started taking off in the early 2000s as insurance plans shifted more costs to patients. Today, nearly one in five prescriptions for privately insured patients uses one of these programs. That’s over $23 billion in savings every year. But here’s the catch: if you’re on Medicare, Medicaid, or another federal program, you’re not eligible. Federal law bans these programs for government-funded patients because they could push people toward more expensive brand drugs instead of cheaper generics.
How Do They Actually Work?
It’s simpler than it sounds. First, you find the program for your drug. Go to the drugmaker’s official website-like Eli Lilly for Humira or Boehringer Ingelheim for Jardiance-and search for “savings” or “patient assistance.” You can also use sites like GoodRx, but always double-check that the offer comes from the manufacturer, not a third party.
Next, you fill out a short online form. You’ll need your insurance info, your doctor’s name, and your prescription details. The system checks your eligibility in seconds. If you qualify, you get a digital card or a code. You don’t need to print anything-most pharmacies accept it via phone or app.
At the pharmacy, your pharmacist enters your insurance and the coupon code. A third-party administrator-like ConnectiveRx or Prime Therapeutics-steps in behind the scenes. They verify you’re eligible, apply the discount, and the drugmaker pays them back. Your out-of-pocket cost drops immediately.
For example, a patient on Jardiance for diabetes paid $562.50 a month before using the manufacturer coupon. After enrollment, their cost dropped to $100. That’s not a one-time deal-it’s monthly, as long as the program is active.
Who Can Use These Programs?
You must have private insurance. That means coverage from an employer, a plan bought through the marketplace, or a spouse’s plan. If you’re on Medicare Part D, Medicaid, VA benefits, or Tricare-you can’t use these coupons. The rules are strict. Pharmacies are required to block the discount if they detect federal insurance.
Some programs also require income verification. For PAPs, you might need to submit tax forms or pay stubs. For copay cards, income checks are rare-but you still need to be insured privately. If you’re uninsured, you might qualify for a PAP, but not a copay card.

What Are the Big Limitations?
These programs aren’t perfect. Three major issues trip people up every day.
- Accumulator Adjustment Programs: Many insurance plans now block manufacturer discounts from counting toward your deductible or out-of-pocket maximum. So even if your copay card cuts your monthly cost from $450 to $100, that $100 doesn’t help you reach your $5,000 deductible. You’re still paying full price toward your plan’s limits. About 87% of large employers use these programs as of 2022.
- Time Limits: Most coupons expire after 12 to 24 months. You have to reapply. Some manufacturers auto-renew, but others don’t. If you forget, your bill jumps back up overnight.
- Caps: There’s usually a yearly limit-between $5,000 and $15,000 per person. Once you hit it, you pay full price for the rest of the year.
One Reddit user shared how their Humira coupon ended without warning. Their monthly cost went from $150 to $1,200. They had no savings left, and their insurance didn’t count the past discounts toward their deductible. They were stuck.
Manufacturer Programs vs. GoodRx and Other Discount Cards
GoodRx, SingleCare, and similar services are different. They’re not made by drugmakers. They’re pharmacy discount cards that negotiate lower cash prices for both brand and generic drugs. You don’t need insurance to use them.
Here’s how they compare:
| Feature | Manufacturer Copay Card | GoodRx/Discount Card |
|---|---|---|
| Who it’s for | Private insurance only | Anyone-insured or not |
| Discount size | 70-85% off | 30-60% off |
| Applies to generics? | No | Yes |
| Counts toward deductible? | Usually not | No |
| Annual cap | Yes ($5K-$15K) | No |
| Expiration | 12-24 months | None |
Manufacturer programs give deeper discounts-but only for brand drugs. GoodRx gives smaller savings but works for generics too. If your drug has a generic version, always check GoodRx first. Sometimes the cash price is lower than your copay after the discount.
What to Do If Your Insurance Blocks the Discount
If your plan has an accumulator program, your copay card won’t help you reach your deductible. That’s a problem. You’ll pay less each month-but you’ll still owe thousands before your insurance kicks in fully.
Here’s what you can do:
- Ask your insurer: “Do you have an accumulator adjustment program?”
- If yes, ask if they’ll waive it for your medication. Some will, especially if you have a chronic condition.
- Call your drugmaker’s patient support line. Some manufacturers offer extra help if you’re stuck in an accumulator plan.
- Check if your state has passed a law banning accumulators. As of 2023, 32 states have.
Some patients switch plans during open enrollment to avoid accumulators. That’s a big move-but worth considering if you’re on a high-cost drug.
How to Avoid Getting Caught Off Guard
These programs can disappear. Companies change them. Insurance rules shift. You need to stay on top of it.
- Set a calendar reminder for 60 days before your coupon expires.
- Check your mail and email from the drugmaker-they often send renewal notices.
- Call your pharmacy monthly to confirm the discount is still being applied.
- Keep a printed copy of your eligibility letter or digital card.
- If your drug gets a generic version, compare prices. Sometimes switching saves more than the coupon.
One patient on a $600/month insulin drug used the manufacturer coupon for two years. When the coupon expired, they switched to the generic version and cut their cost to $35. That’s the new federal cap for Medicare-but even private insurers are starting to follow.
Why These Programs Exist-and the Debate Around Them
Drugmakers say these programs help patients afford life-saving meds. And they do. But they also serve a business purpose. Studies show copay cards increase brand drug sales by 60% or more. They keep people on expensive drugs instead of switching to cheaper generics.
Experts like Dr. Robin Feldman argue this distorts the market. When patients pay less upfront, they don’t feel the true cost. That means drugmakers can keep prices high, and insurers end up paying more later. It’s a cycle.
Meanwhile, PhRMA, the drug industry group, says these programs are essential lifelines. Without them, many patients would skip doses or quit treatment.
The truth? Both sides are right. These programs help people today-but they may make drug prices worse over time.
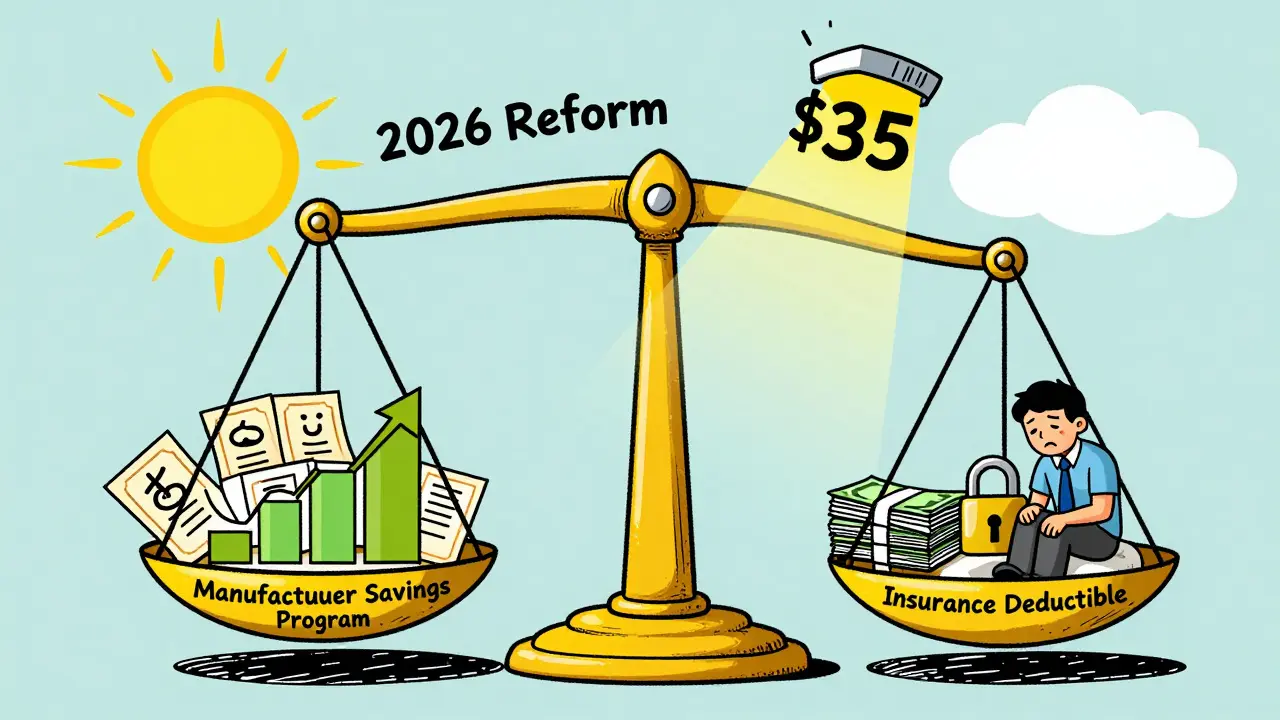
What’s Changing in 2026?
The 2022 Inflation Reduction Act capped insulin at $35 for Medicare patients. That’s already reducing reliance on manufacturer coupons for insulin. Other drugs may follow.
Legislation like the 2023 Fair Deal for Patients Act could force manufacturers to let their discounts count toward deductibles. If that passes, the whole system changes.
For now, these programs are still your best bet-if you qualify. But don’t assume they’ll be around forever. Use them wisely, track your usage, and always have a backup plan.
Can I use a manufacturer savings program if I have Medicare?
No. Federal law prohibits drugmakers from offering copay cards or coupons to Medicare or Medicaid patients. This is to prevent financial incentives that could push beneficiaries toward more expensive brand drugs. If you’re on Medicare, you can use GoodRx or other pharmacy discount cards, but not manufacturer-specific coupons.
Do these programs work with all pharmacies?
Most major chains like CVS, Walgreens, Rite Aid, and Walmart accept them. Smaller independent pharmacies may not have the system set up to process the discounts. Always call ahead or check the manufacturer’s website for a list of participating pharmacies. If your local pharmacy doesn’t accept it, you can often get the discount at a nearby chain.
What if my copay card stops working suddenly?
First, check if your coupon expired. Most last 12-24 months. If it’s still active, contact the drugmaker’s patient support line immediately. They can often reissue your card or explain why it was blocked. Also, call your pharmacy-they may see an error on their end. If your insurance changed or your plan has an accumulator program, that could also be the cause.
Can I use more than one savings program at the same time?
No. You can only use one discount per prescription. You can’t stack a manufacturer coupon with a GoodRx card. The pharmacy system will only accept one. Always choose the one that gives you the lowest price. Use GoodRx to compare prices first, then decide which discount to apply.
Are there alternatives if I don’t qualify for a manufacturer program?
Yes. If you’re on Medicare, use GoodRx or RxSaver. If you have low income, check if you qualify for a Patient Assistance Program (PAP) directly from the drugmaker-they often have income-based free drug programs. Nonprofits like NeedyMeds and the Patient Access Network Foundation also offer grants for high-cost medications. Your pharmacist can help you find these options.


Mohammed Rizvi
January 24, 2026 AT 14:13This system is a cleverly disguised tax on the poor. Drug companies get to play hero while keeping prices sky-high, and we’re supposed to be grateful for the crumbs. The real scandal isn’t that these programs exist-it’s that they’re the only option left.
Skye Kooyman
January 25, 2026 AT 01:15I used a Jardiance card for 18 months. When it expired, my bill jumped from $80 to $580. No warning. No email. Just a receipt that looked like a ransom note.
rasna saha
January 26, 2026 AT 01:38For anyone struggling with this-reach out to your pharmacist. They know all the hidden programs and can often connect you with nonprofit aid. You’re not alone, and there are people who want to help.
TONY ADAMS
January 26, 2026 AT 10:03Yo so I got my Humira coupon cut off last month and now I’m paying $1200? That’s wild. My mom’s on Medicare so she can’t even use these things. Why do they even make these programs if they’re gonna yank them like that? Feels like a trap.
shivam utkresth
January 27, 2026 AT 05:48As someone from India where insulin costs $5 a vial, seeing Americans fight over $100 copays is surreal. But I get it-this isn’t just about price, it’s about dignity. These programs are a Band-Aid on a bullet wound. Still, if they keep someone alive today, I won’t judge them for using it.
Napoleon Huere
January 29, 2026 AT 04:48These programs are a microcosm of late-stage capitalism: personalized relief packaged as systemic generosity. The drugmakers don’t care if you hit your deductible-they care if you stay hooked on their brand. The discount isn’t altruism, it’s behavioral engineering. We’re being conditioned to accept high prices because we’re told we’re getting a deal. But the deal is rigged. The real cost isn’t paid at the counter-it’s paid in inflation, in insurance premiums, in the erosion of trust. And no one’s auditing that ledger.
Curtis Younker
January 29, 2026 AT 23:13Hey everyone, I just want to say-you’re not alone in this! I’ve been using these savings programs for my diabetes meds for over three years now, and honestly, they’ve saved my life. I was working two jobs just to afford my prescriptions before I found the manufacturer coupon. Now I can actually sleep at night knowing I can afford my meds. And yes, I set reminders for renewal, I check my email, I call the pharmacy every month-because this stuff matters. Don’t give up! There’s always a way, and if you need help figuring it out, I’m happy to walk you through it. You’ve got this!
Uche Okoro
January 30, 2026 AT 15:44The structural inefficiencies inherent in the pharmaceutical supply chain are exacerbated by the proliferation of third-party administrative intermediaries. The accumulator adjustment programs represent a form of moral hazard mitigation by payers, yet the absence of regulatory alignment between federal statutes and private sector incentives creates perverse outcomes. The utilization of manufacturer copay cards, while statistically significant in reducing out-of-pocket expenditure, concurrently distorts price elasticity and suppresses generic substitution dynamics, thereby entrenching monopolistic pricing paradigms. This is not a patient assistance mechanism-it is a market distortion vector.
Aurelie L.
January 31, 2026 AT 06:53My card expired. They didn’t tell me. Now I owe $2,000. And my doctor says ‘just switch.’ Like it’s that easy.
George Rahn
January 31, 2026 AT 16:19Let us not be naive. These programs are not gifts from benevolent corporations-they are strategic instruments of economic warfare waged against the American public by oligopolistic entities that have captured our legislative apparatus. The very notion that a private entity may dictate access to essential medicine under the guise of compassion is a moral abomination. The Constitution guarantees life, liberty, and the pursuit of happiness-not a coupon. We must demand universal access to affordable pharmaceuticals, not charity from corporations that profit from our suffering. This is not healthcare. This is extortion with a smile.