When a patient walks into your office asking why their prescription now looks different, or complains that their blood pressure isn’t as controlled as before, it’s not just a packaging issue-it’s a clinical one. Providers across the U.S. have been navigating the rise of generic medications for decades, and the real-world experiences aren’t always what you’d expect from a regulatory checklist. The FDA says generics are bioequivalent. The data says they work. But the stories from clinics, hospitals, and pharmacies tell a more complicated picture.
Generics Are the Norm, But Not Always Seamless
By 2023, generic medications made up 90% of all prescriptions filled in the U.S. That’s not a small shift-it’s the new standard. And yet, for many providers, the transition isn’t as smooth as the numbers suggest. Take statins, for example. Atorvastatin, the generic version of Lipitor, is prescribed daily in millions of cases. Most patients switch without issue. Blood pressure drops. Cholesterol levels improve. Cost savings are huge. A 2006-2007 Medicaid analysis showed that eliminating consent requirements for just three drugs-atorvastatin, clopidogrel, and olanzapine-could have saved over $100 million in one year. That’s the win everyone talks about.
But then there’s the flip side. A patient on brand-name lamotrigine for epilepsy has been seizure-free for three years. The pharmacy substitutes it with a generic version. Within weeks, they’re back in the ER with a breakthrough seizure. This isn’t rare. Case reports from neurologists across the country document this exact pattern. The FDA’s Orange Book lists these generics as AB-rated-therapeutically equivalent. But for drugs with a narrow therapeutic index, like antiepileptics, even small differences in absorption can matter. The American College of Neurology doesn’t mince words: they recommend against mandatory substitution without explicit consent from both patient and provider.
Therapeutic Equivalence Isn’t Always Black and White
The FDA’s therapeutic equivalence ratings-AB, BX, and others-are meant to guide substitution. AB means the generic is interchangeable. BX means it’s not. But here’s the catch: those ratings don’t always reflect real-world outcomes. In 2016, the FDA reviewed two generic versions of Concerta after a flood of complaints about reduced effectiveness. Lab tests, adverse event logs, and expert reviews led to those generics being downgraded from AB to BX. That’s rare. Most generics never get that level of scrutiny. But it shows the system isn’t perfect.
For drugs like warfarin, cyclosporine, or levothyroxine, providers often take extra steps. Many write “dispense as written” on prescriptions. Others track which manufacturer’s version a patient is on, because switching between different generic manufacturers-even if they’re all AB-rated-can cause instability. One cardiologist in Boston told me about a patient who went from one generic levothyroxine to another, then to a third, over six months. Her TSH levels jumped from 2.1 to 7.8. It took three months to stabilize again. No one had told her the pill looked different because the manufacturer changed. She thought she was still on the same drug.
Who Decides? The Role of Patient Trust
It’s not just about the science. It’s about perception. A 2024 study in Greece found that 68% of women followed their doctor’s advice to switch to generics. Only 64% of men did. Why? The same study showed patients who had a direct conversation with their provider were far more likely to accept the switch. That’s the key. A 10-minute explanation about how generics are tested, why they’re cheaper, and that the active ingredient is identical can dramatically improve adherence.
But not all providers are comfortable with that conversation. Some avoid it, fearing patients will refuse. Others assume patients will panic if they hear the word “generic.” That’s a mistake. A 2001-2003 study found patients who started on generics had 13% better adherence than those on brand-name drugs-likely because they could afford them. The problem isn’t the drug. It’s the messaging. When a pharmacist hands over a pill in a plain white bottle and says, “This is the same as your old one,” patients hear: “This is cheaper. Maybe it’s worse.”
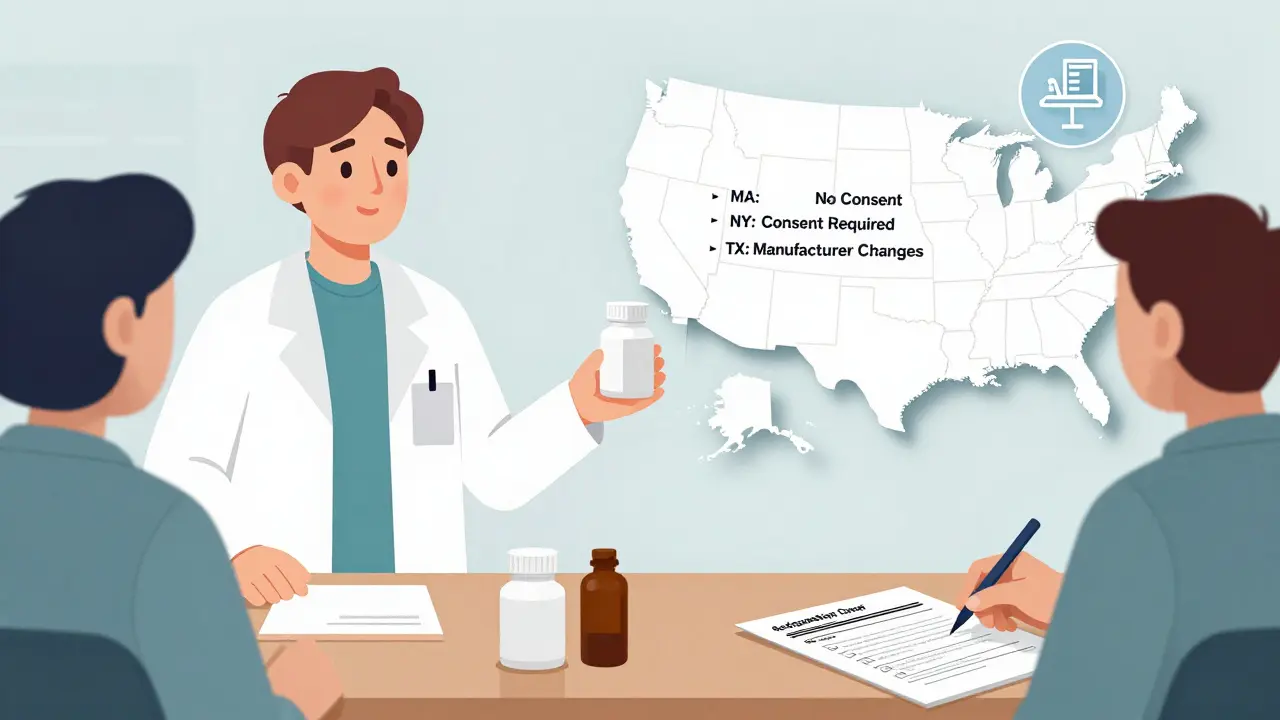
State Laws Create a Patchwork of Rules
Here’s where it gets messy. In 19 states, pharmacists can substitute generics without telling the patient. In seven states and Washington, D.C., they must get the patient’s consent first. In 24 states, pharmacists aren’t protected from liability if something goes wrong after substitution. That means some pharmacists refuse to switch drugs unless the doctor says so. Others avoid substitution entirely to avoid legal risk. The result? A patient in Massachusetts might get a generic without knowing. A patient in New York might be asked to sign a form. A patient in Texas might get a different generic every time they refill, because the pharmacy’s contract with their wholesaler changes.
Electronic health records (EHRs) are supposed to help. Many now show therapeutic equivalence codes. But not all systems are updated. Some don’t flag BX-rated drugs at all. Others don’t show which generic manufacturer the patient is on. Providers end up relying on memory, paper records, or patient self-reporting-which is unreliable.
Authorized Generics: The Hidden Middle Ground
There’s a lesser-known category called authorized generics. These are the exact same pills as the brand-name drug, just sold without the brand logo. Made by the original manufacturer. Same factory. Same packaging. Same inactive ingredients. The only difference? The price. They’re cheaper than the brand, but often more expensive than regular generics. Why? Because they’re not competing with other manufacturers.
For providers treating high-risk patients-those on immunosuppressants after transplant, or those with bipolar disorder on lithium-authorized generics are often the preferred choice. A 2019 JAMA Internal Medicine study found no significant difference in hospitalization or discontinuation rates between authorized generics and regular generics. But patients reported more confidence in them. Why? Because they looked and felt familiar. The same pill, just a different label.

What’s Changing Now?
The Inflation Reduction Act of 2022 is pushing Medicare Part D toward even stricter generic-first policies. By 2025, experts predict generic substitution rates will rise 5-7 percentage points. That’s good for costs. But it also means more patients will be switched, often without a conversation. The FDA is also stepping up scrutiny of complex generics-like inhalers, topical creams, and injectables-where bioequivalence is harder to prove. In 2023, they released draft guidance on formulation development to address those gaps.
Meanwhile, real-world data is starting to supplement lab tests. The FDA’s Sentinel Initiative tracks outcomes from millions of prescriptions. Machine learning models are being tested to predict which patients are most likely to have trouble switching. One 2024 Greek study used a Random Forest algorithm to identify that patients with lower education, no prior generic use, or recent hospitalizations were 3x more likely to resist substitution. That’s the future: personalized risk assessments, not blanket rules.
The Bottom Line for Providers
Generics work. For most people, most of the time. But they’re not all the same. And switching isn’t just a pharmacy decision-it’s a clinical one. Providers who treat patients on narrow therapeutic index drugs need to be vigilant. Those who manage chronic conditions like hypertension, diabetes, or epilepsy should track which version their patients are on. And everyone should talk to their patients. Not just about cost. About consistency. About why a pill might look different but still do the same job.
The data says generics are safe. The stories say they’re not always simple. The best approach? Know the drug. Know the patient. And don’t assume equivalence just because the label says so.
Are generic medications really as effective as brand-name drugs?
For the vast majority of drugs, yes. The FDA requires generics to prove they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. Studies show no meaningful difference in outcomes for drugs like statins, ACE inhibitors, or antidepressants. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or antiepileptics-even small variations can matter. That’s why some providers avoid switching these without careful monitoring.
Why do some patients say generics don’t work for them?
Sometimes it’s psychological-patients associate the brand with effectiveness. Other times, it’s real. Switching between different generic manufacturers can change inactive ingredients, pill size, or absorption rates, especially with complex formulations. In epilepsy, for example, multiple switches have been linked to breakthrough seizures. A patient who’s stable on one generic may react poorly to another, even if both are FDA-approved.
Can pharmacists substitute generics without my doctor’s approval?
It depends on your state. In 19 states, pharmacists can substitute generics automatically. In 7 states and Washington, D.C., they must get your consent first. Some states also require pharmacists to inform you if the generic comes from a different manufacturer than your last refill. Always check your local laws-and ask your pharmacist if you’re unsure.
What’s the difference between a generic and an authorized generic?
A regular generic is made by a different company than the brand. An authorized generic is made by the original brand manufacturer but sold under a different label, usually at a lower price. It’s the exact same pill, same factory, same ingredients. Many providers prefer authorized generics for high-risk patients because they eliminate the uncertainty of switching manufacturers.
Should I avoid generics if I’m on a critical medication?
Not necessarily. But for drugs like antiepileptics, immunosuppressants, or blood thinners, it’s wise to be cautious. Ask your provider if your specific drug has a history of substitution issues. If you’ve been stable on a brand or a specific generic, ask to stay on it. You can also request an authorized generic or ask your pharmacist to keep you on the same manufacturer each time.