Sevelamer hydrochloride — what it does and who needs it
Did you know sevelamer hydrochloride is a phosphate binder used mainly in people with chronic kidney disease (CKD) on dialysis? When kidneys can't remove phosphate, levels rise and that can harm bones and blood vessels. Sevelamer grabs phosphate in the gut so less is absorbed, helping keep blood phosphate in range without adding extra calcium.
How it works and who should take it
Sevelamer is not a pill that fixes kidneys — it works inside the gut. You take it with meals so it can bind phosphate from food right away. Doctors usually prescribe it for patients on hemodialysis or peritoneal dialysis with high phosphate levels. It’s a go-to when you want to avoid calcium-based binders (like calcium acetate) because those can raise calcium and increase the risk of vascular calcification.
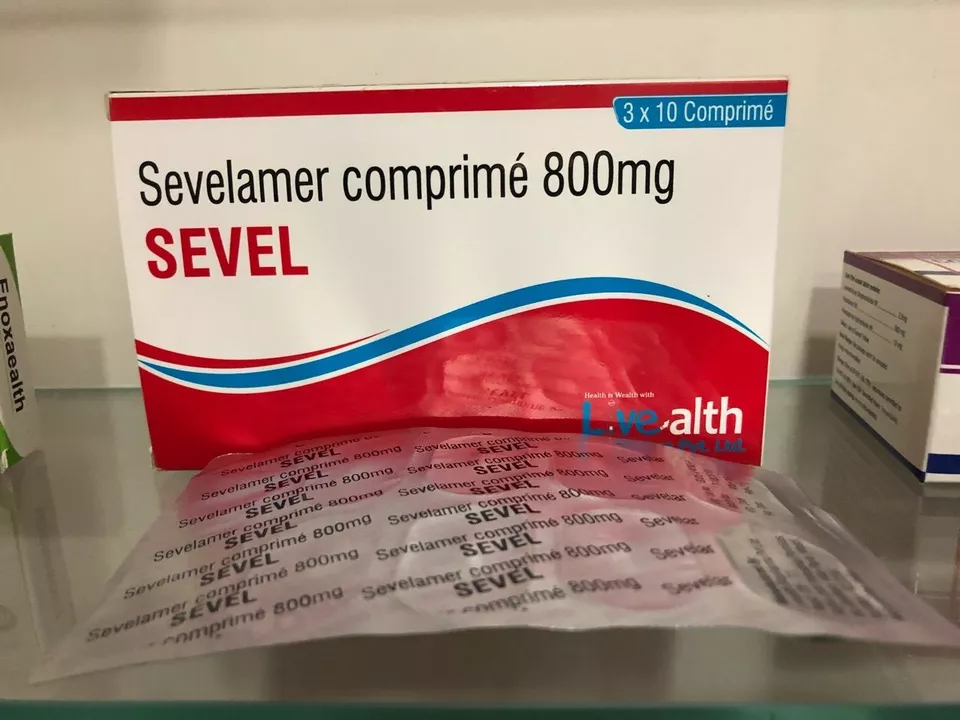
There are two common forms: sevelamer hydrochloride and sevelamer carbonate. Hydrochloride can sometimes lower bicarbonate and mildly affect acid-base balance, so your care team will watch blood tests. You’ll need regular lab checks — phosphate, calcium, parathyroid hormone (PTH), and bicarbonate — while on treatment.
How to take it, side effects, and practical tips
Take sevelamer with food. If you forget a dose, take it with your next meal — don’t double up. It comes as tablets, chewable tablets, or powder to mix. Chew or mix as the label says; swallowing whole tablets reduces effectiveness.
Common side effects are mostly gastrointestinal: nausea, bloating, gas, constipation, or diarrhea. Constipation is frequent — drinking enough fluids (as allowed by your kidney team), adding fiber if safe, or using stool softeners can help. Serious problems are rare but include severe bowel obstruction in people with preexisting GI issues; tell your doctor about any severe belly pain.
Drug interactions matter. Sevelamer can bind other oral meds and reduce their absorption — examples include some antibiotics, thyroid medicine, and immunosuppressants. A simple rule: give other oral meds at least 1 hour before or 3 hours after sevelamer when possible. Always check with your pharmacist or doctor before starting a new drug.
Alternatives to sevelamer include calcium-based binders, lanthanum carbonate, and iron-based binders. Each has pros and cons: calcium binders can raise calcium, lanthanum is effective but pricier, and iron-based binders add iron. Your care team will pick the best one for your labs and overall health.
Quick checklist for patients: take with meals, don't crush chewables unless directed, watch for constipation, separate other meds to avoid interactions, and keep up with blood tests. If you notice unusual symptoms—severe stomach pain, persistent vomiting, or signs of low phosphate—contact your clinic right away.
Sevelamer hydrochloride is a practical tool for controlling phosphate in dialysis patients. With the right dosing, monitoring, and simple habits, it can protect your bones and blood vessels while avoiding extra calcium load.
Frequently asked questions about Sevelamer Hydrochloride
- by Colin Edward Egan
- on 12 May 2023
As a blogger, I've come across many questions about Sevelamer Hydrochloride, so I wanted to share a quick summary with you all. Sevelamer Hydrochloride is a phosphate binder, commonly prescribed to patients with chronic kidney disease to help control their blood phosphorus levels. It works by binding to phosphate in the food we eat, preventing its absorption into the bloodstream. This medication is usually taken with meals and comes in tablet or powder form. Remember to always consult your healthcare professional before starting any new medication, as they can provide you with the most accurate information regarding dosage and potential side effects.
