Osteoporosis in Pregnancy: Risks, Prevention, and Treatment
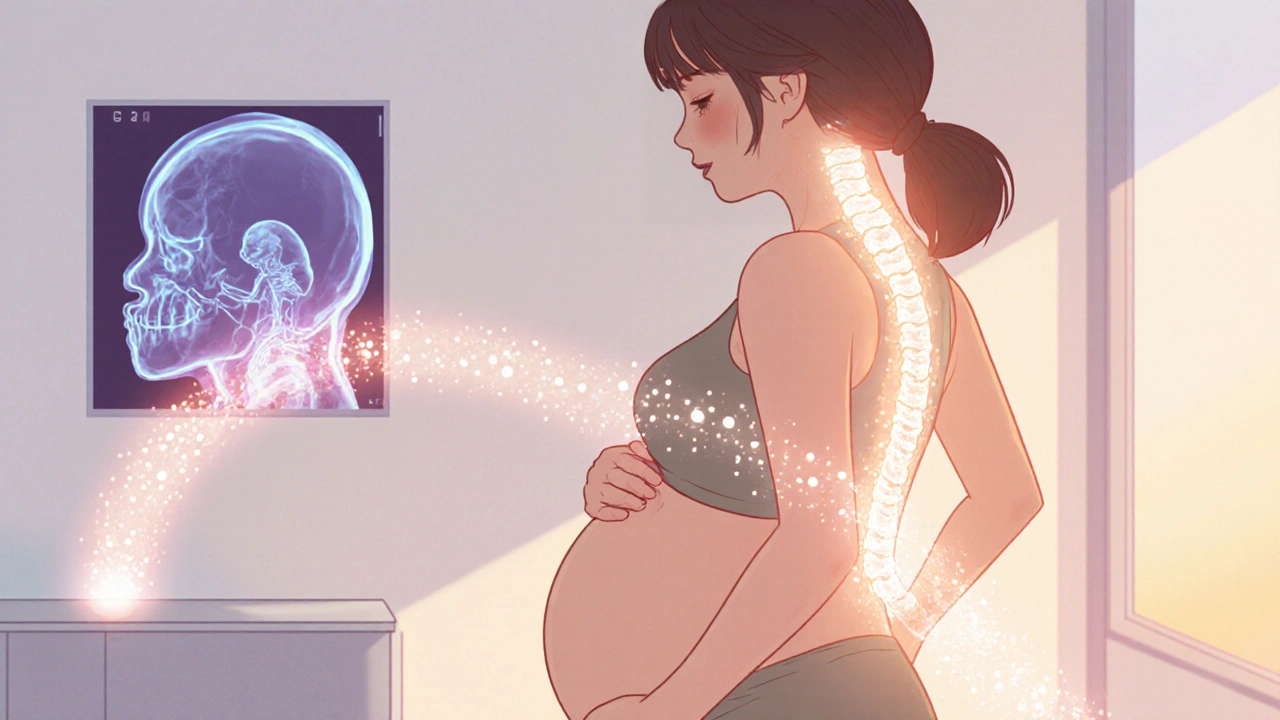
When working with osteoporosis during pregnancy, a condition where a pregnant woman's bone density drops below normal, raising fracture risk for the mother and affecting fetal calcium supply. Also known as pregnancy‑related osteoporosis, it demands careful attention because the body is already juggling hormonal shifts, extra weight, and the baby's nutritional needs. Managing the condition requires adequate calcium intake, sufficient vitamin D levels, and a thoughtful look at medications such as bisphosphonates. If you’re searching for reliable info on osteoporosis pregnancy, you’ve come to the right place.
Why does bone loss sneak in during pregnancy? The hormone progesterone relaxes ligaments, while estrogen, which normally protects bone, drops after the first trimester. Add a diet low in calcium or limited sun exposure, and the body starts pulling calcium from the skeleton to keep the developing baby’s teeth and bones strong. Women with a history of low bone mass, smoking habits, or chronic steroid use are especially vulnerable. This trio—hormonal change, nutrient deficit, and preexisting risk—creates the perfect storm for reduced bone mineral density.
Practical Prevention Strategies
Prevention starts with what’s on the plate. Dairy products, fortified plant milks, leafy greens, and almonds are quick ways to boost calcium. Pair those foods with safe sunlight exposure or a prenatal vitamin that contains vitamin D; together they enhance calcium absorption and support bone remodeling. Weight‑bearing activities like walking, low‑impact aerobics, or prenatal yoga add mechanical stimulus that signals the body to maintain bone strength. A simple semantic triple: adequate calcium intake enables healthy bone formation, while vitamin D facilitates calcium absorption.
When diet alone falls short, supplementation becomes a smart move. Most obstetricians recommend 1,000–1,200 mg of calcium and 600–800 IU of vitamin D daily for pregnant women at risk of osteoporosis. Blood tests can confirm levels and guide dosage, ensuring you don’t overshoot and cause kidney stones. Keeping a weekly log of food, supplements, and activity helps both you and your healthcare provider spot gaps early.
Medication choices need extra caution. Bisphosphonates, the go‑to drugs for postmenopausal osteoporosis, stick to bone for years and could affect the newborn’s developing skeleton, so they are generally avoided during pregnancy. Safer alternatives include calcium + vitamin D combos, and in severe cases, a short course of intravenous calcium under strict medical supervision. Some specialists also consider teriparatide, a hormone‑like drug that builds bone, but only after delivery and with lactation in mind.
The baby’s health is tied to the mother’s bone status. A well‑balanced calcium‑vitamin D supply ensures the fetus builds a strong skeletal framework without draining the mother’s reserves. After delivery, the sudden drop in pregnancy hormones can spike bone loss, so continued nutrition and gentle exercise remain vital. Breastfeeding adds another calcium demand, making post‑partum follow‑up essential for long‑term maternal bone health.
With these insights, you’re equipped to recognize the warning signs, adopt preventive habits, and discuss safe treatment options with your provider. Below you’ll find a curated list of articles that dive deeper into each aspect—risk factors, diet plans, supplement guidelines, and the latest research on medication safety during pregnancy. Explore the collection to arm yourself with the knowledge you need for a healthy pregnancy and strong bones afterward.
Osteoporosis and Pregnancy: Essential Guide for Expectant Moms
- by Colin Edward Egan
- on 19 Oct 2025
Learn how pregnancy impacts bone health, identify risk factors, and discover safe nutrition, exercise, and medication tips to protect against osteoporosis.
