Hyponatremia prevention: how to protect your sodium and avoid trouble
Low blood sodium (hyponatremia) can sneak up fast. You don’t need medical school to make a big difference—small, practical changes cut your risk. Below I’ll walk you through who should be careful, what to watch for, and real steps to keep your sodium in a safe range.
Who’s at risk and warning signs
Some people are more likely to get hyponatremia: older adults, people on certain medicines (like some diuretics, SSRIs, or seizure drugs), athletes who drink a lot of plain water during long events, and anyone with conditions that cause the body to hold water (heart, liver, kidney problems, or SIADH). Hospital patients who get large amounts of IV fluids can also develop it.
Watch for nausea, headache, confusion, dizziness, muscle cramps, and feeling very tired. Severe cases cause seizures or loss of consciousness—those are emergencies. If you’re in a high-risk group and notice these signs, call a doctor or go to the ER.
Practical prevention tips
1) Drink to thirst, not to a schedule. For most people, thirst is a reliable guide. For long workouts or races, replace fluids with a balanced sports drink that contains sodium and other electrolytes rather than plain water.
2) Talk with your doctor about your medications. If you take diuretics, SSRIs, or other drugs linked to hyponatremia, ask whether your dose or choice of drug can be adjusted and whether you need periodic sodium checks.
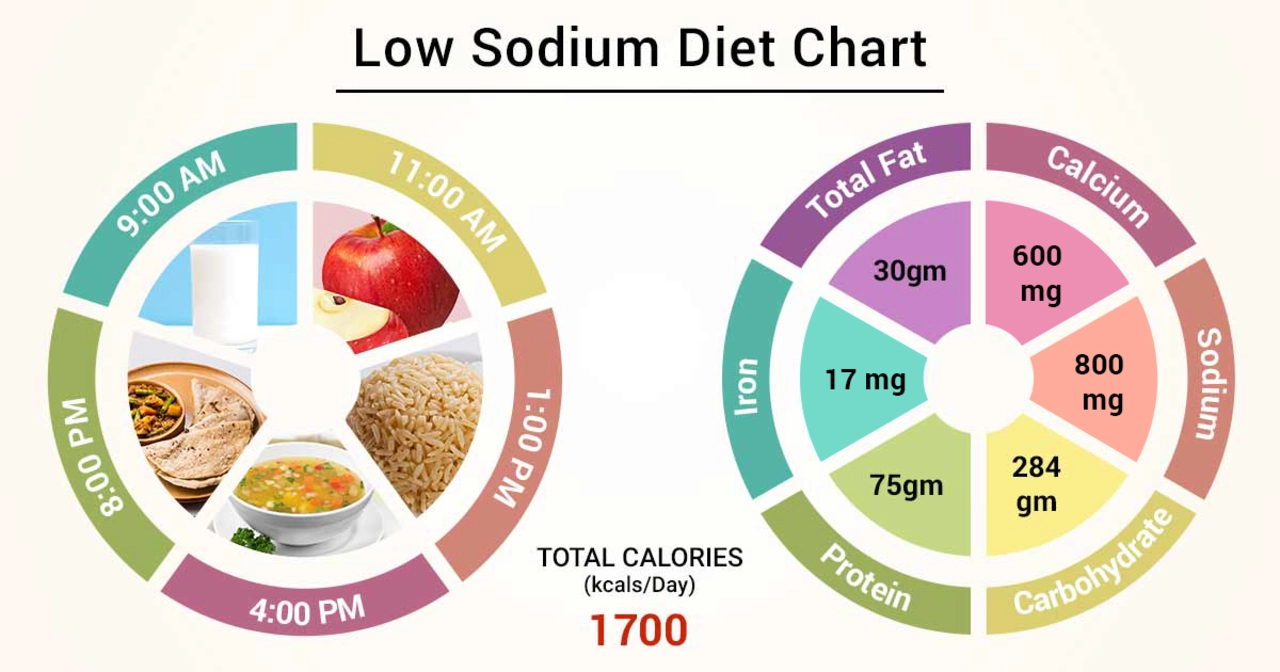
3) Be careful with “low-sodium” diets only if your clinician told you to restrict salt. Some people who cut salt too much and then drink large amounts of water can lower blood sodium. Follow personalized advice from your healthcare provider.
4) For older adults, check labs regularly. Age changes how the body handles water and sodium. Simple blood tests can catch early drops in sodium before symptoms start.
5) In hospitals and clinics, ask what IV fluids you’re getting. If you’re at risk, point out that hypotonic (very low-sodium) IV fluids can worsen hyponatremia. Staff can choose isotonic solutions when appropriate.
6) During long endurance events, use a hydration plan that includes electrolytes or salty snacks. Some athletes match fluid intake to sweat losses; others use salt tablets under guidance from a sports medicine pro.
7) Treat underlying conditions that cause water retention—like heart failure or liver disease—under medical care. Managing the root cause reduces the chance of hyponatremia repeated episodes.
If you suspect hyponatremia, don’t try to fix it yourself with salt loading or extreme fluid restriction—those moves can be dangerous without supervision. Quick medical evaluation and an appropriate plan are the safest route. Simple habits—drink sensibly, review meds, and check labs when needed—do most of the work in preventing low sodium.
The Role of Diet in Preventing and Managing Hyponatremia
- by Colin Edward Egan
- on 15 May 2023
In my latest blog post, I discussed the role of diet in preventing and managing hyponatremia, a condition characterized by low sodium levels in the blood. I emphasized the importance of maintaining a balanced diet, which includes consuming adequate amounts of sodium to help regulate fluid balance in the body. In addition, I explored how drinking enough water, avoiding excessive consumption of sodium-rich foods, and being mindful of medications can help prevent and manage this condition. By paying attention to our diet, we can greatly reduce our risk of developing hyponatremia and lead a healthier life. Stay tuned for more tips on maintaining a balanced diet and overall well-being!
