Cholesterol Treatment Decision Tool
How This Tool Works
This tool helps you determine which cholesterol treatment option may be more appropriate for your situation based on factors like your current LDL levels, medical history, side effect tolerance, and personal preferences. The recommendations are based on guidelines from the American Heart Association and clinical evidence from the article.
Your results will appear here after clicking the calculate button.
When it comes to lowering cholesterol, two main options dominate: statins and PCSK9 inhibitors. Both work to reduce LDL (bad) cholesterol, but they’re fundamentally different in how they work, how they’re taken, and what side effects they cause. If you’ve been told your cholesterol is too high and you’re trying to decide between these two, you’re not alone. Millions of people face this choice every year - and the right answer depends on your health, your tolerance, and your budget.
How Statins Work - and Why They’re Still the Go-To
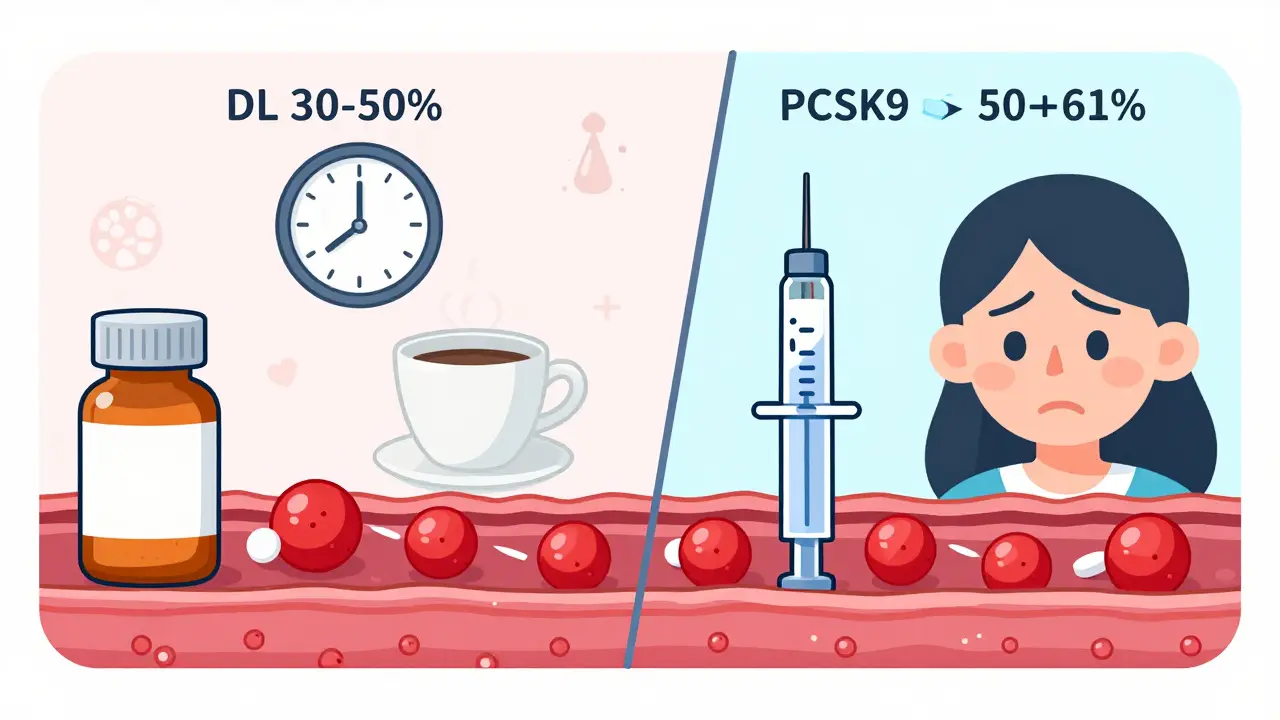
Statins have been around since the late 1980s. They’re pills you take daily, and they work by blocking an enzyme in your liver called HMG-CoA reductase. That enzyme is responsible for making cholesterol. When you slow it down, your liver pulls more LDL out of your blood to make up for the loss. The result? A 30% to 50% drop in LDL cholesterol for most people. What makes statins so popular isn’t just how well they work - it’s how long we’ve known they work. Decades of data show they cut heart attacks, strokes, and deaths in people with heart disease. That’s why the American Heart Association and the American College of Cardiology still say statins are the first-line treatment for almost everyone with high cholesterol or heart disease risk. They’re also cheap. Generic versions like atorvastatin and simvastatin cost as little as $4 to $10 a month. For many people, that’s the biggest reason they stick with them.What About the Side Effects?
Not everyone tolerates statins well. About 5% to 10% of people experience muscle pain, stiffness, or weakness - a condition called statin-associated muscle symptoms. For some, it’s mild. For others, it’s bad enough to stop taking the drug entirely. A 2023 study in Mayo Clinic Proceedings found that nearly one-third of people who quit statins blamed muscle pain. Other complaints? Memory fog and fatigue. These aren’t common, but they’re real enough that patients report them on review sites like Drugs.com. About 18% of negative statin reviews mention brain fog. The science isn’t clear if statins directly cause this, but patients swear they feel different after starting them. There’s another risk: hemorrhagic stroke. Research from UCLA in 2023 showed statins increase the risk of this type of stroke by 22% in certain people - especially those with high blood pressure or a history of bleeding in the brain. It’s rare, but it’s a real trade-off.PCSK9 Inhibitors: The New Kid on the Block
PCSK9 inhibitors came onto the scene in 2015. Unlike statins, they’re not pills. They’re injections you give yourself under the skin - either every two weeks or once a month. Two drugs dominate this class: alirocumab (Praluent) and evolocumab (Repatha). Here’s how they work: PCSK9 is a protein that tells your liver to destroy LDL receptors. Without enough receptors, LDL stays in your blood. PCSK9 inhibitors block that protein, so your liver keeps more receptors alive. More receptors = more LDL pulled out of your bloodstream. The result? A 50% to 61% drop in LDL cholesterol - significantly more than even high-dose statins. In the FOURIER trial, evolocumab cut LDL by 59%. In the ODYSSEY trial, alirocumab dropped it by 61%. Some patients on both a statin and a PCSK9 inhibitor see drops over 75%.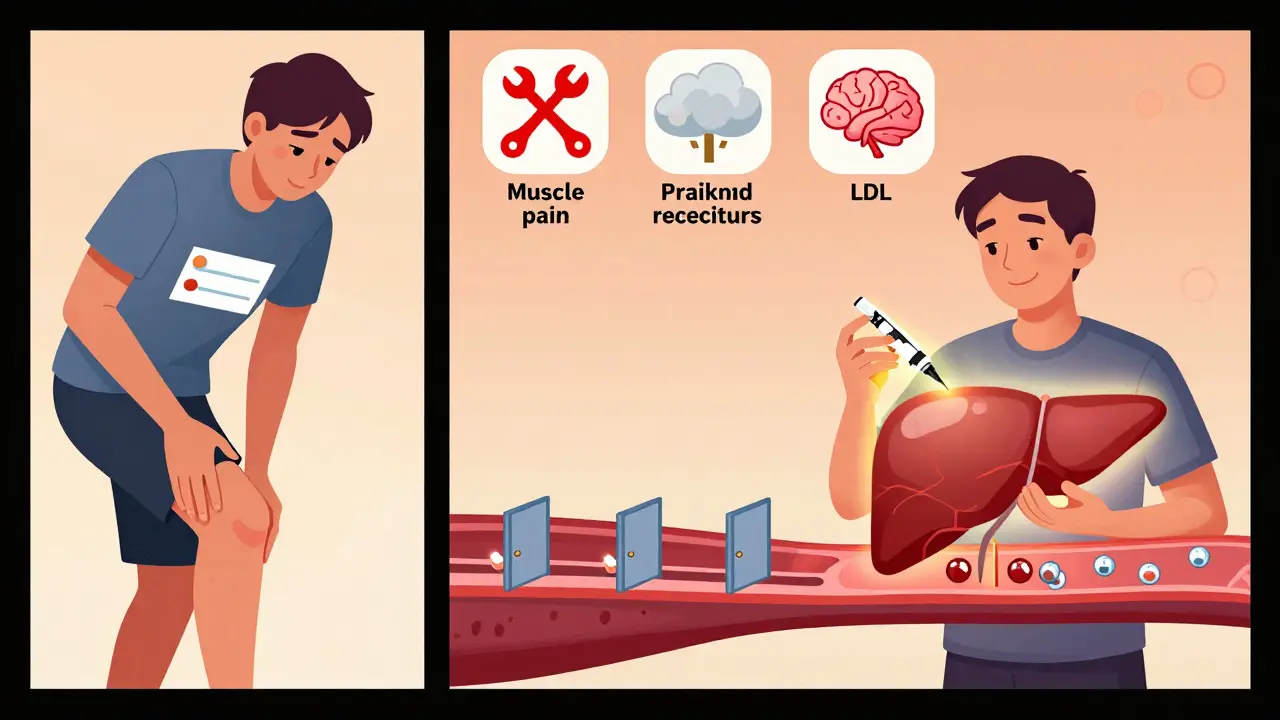
Side Effects of PCSK9 Inhibitors
The biggest advantage? Almost no muscle pain. In fact, 79% of patients who switched from statins to PCSK9 inhibitors on Drugs.com said they no longer had muscle issues. That’s a game-changer for people who can’t tolerate statins. They also don’t raise the risk of hemorrhagic stroke. Across 36 clinical trials, no link was found between PCSK9 inhibitors and this type of stroke - a big plus for people with high blood pressure or a history of bleeding. But they’re not side-effect free. The most common complaint? Injection site reactions. Redness, itching, or bruising at the spot where you inject. It’s usually mild and goes away. A smaller group - about 41% of users - say they feel anxious about giving themselves shots. For some, that’s enough to quit. There’s also the cost. A full year of PCSK9 inhibitors can run $5,000 to $14,000. Even with insurance, copays can hit $300 a month. That’s why insurers require proof you’ve tried and failed on statins - or can’t take them at all - before approving coverage.Who Gets PCSK9 Inhibitors - and Why?
These drugs aren’t for everyone. They’re reserved for specific groups:- People with familial hypercholesterolemia - a genetic condition that causes extremely high LDL from birth
- Patients with established heart disease (like a past heart attack or stroke) whose LDL stays above 70 mg/dL even on maximum statin therapy
- Those who can’t take statins due to muscle pain or other side effects
Cost vs. Benefit: Is It Worth It?
The price tag is the biggest barrier. Statins cost pennies. PCSK9 inhibitors cost thousands. But cost isn’t just about the pill - it’s about outcomes. A 2024 study in the Journal of the American College of Cardiology found that for very high-risk patients - those with heart disease and LDL above 100 - PCSK9 inhibitors cost about $45,000 per quality-adjusted life year gained. That’s within the range many health systems consider cost-effective. In other words: if you’re at high risk for another heart attack or stroke, and statins aren’t enough, the long-term savings from avoiding hospitalizations and procedures can outweigh the drug’s price. Still, many patients can’t afford it. Insurance denials are common. One Reddit user wrote: “I got approved for Repatha after 11 appeals and 3 months of waiting. I cried when I got the email.”
How They’re Taken - Practical Differences
Statins: Take one pill every day. No training needed. Just swallow and forget. PCSK9 inhibitors: You need to learn how to inject. Most patients get trained by a nurse or pharmacist. The ODYSSEY COMFORT trial found 85% of people mastered the technique after three tries. The devices are simple - pen-like injectors with hidden needles. Still, the idea of poking yourself every few weeks is intimidating for some. Storage matters too. PCSK9 inhibitors must be kept refrigerated. You can’t leave them on the counter like your statin pill bottle.What’s Next? New Options on the Horizon
The field is changing fast. In 2021, the FDA approved inclisiran (Leqvio), a PCSK9-targeting drug that only needs two shots a year. That’s a big deal for people who hate frequent injections. Even more exciting? Oral PCSK9 inhibitors are in clinical trials. Merck’s MK-0616, tested in mid-2024, lowered LDL by 60% - just like the injectables - but as a pill. If approved, it could change everything. There’s also bempedoic acid (Nexletol), a non-statin pill that works differently and has fewer muscle side effects. It’s often used alongside statins when they’re not enough.Final Thoughts: Which One’s Right for You?
If you’re new to cholesterol treatment and have moderate risk, statins are still the best place to start. They’re proven, cheap, and effective. If you’ve tried statins and can’t tolerate them - or your LDL is still too high despite maximum doses - PCSK9 inhibitors are a powerful alternative. They’re more effective, safer for your muscles and brain, and they don’t raise stroke risk like statins can. The decision isn’t just medical. It’s financial. It’s emotional. It’s about your daily life. Talk to your doctor about your goals: Do you want the lowest possible LDL? Are you worried about muscle pain? Can you afford the cost? Can you handle injections? There’s no one-size-fits-all answer. But with the right information, you can choose the path that fits your body - and your life.Can you take PCSK9 inhibitors instead of statins?
Yes - but only under specific conditions. PCSK9 inhibitors are not first-line treatments. Doctors usually prescribe them only if you can’t tolerate statins, or if your LDL remains too high despite taking the highest safe dose of a statin. They’re especially recommended for people with familial hypercholesterolemia or established heart disease.
Do PCSK9 inhibitors cause muscle pain like statins?
No, PCSK9 inhibitors do not cause statin-like muscle pain. In fact, most patients who switch from statins to PCSK9 inhibitors report their muscle symptoms disappear. Clinical trials show muscle-related side effects are no more common with PCSK9 inhibitors than with a placebo.
Are PCSK9 inhibitors better than statins for lowering LDL?
Yes, for LDL reduction alone, PCSK9 inhibitors are more effective. They typically lower LDL by 50-61%, compared to 30-50% for high-intensity statins. When used together, the combination can reduce LDL by over 75%. But statins have broader benefits - including reducing inflammation and stabilizing artery plaques - which PCSK9 inhibitors don’t directly affect.
Why are PCSK9 inhibitors so expensive?
They’re biologic drugs made using living cells, which makes them much harder and costlier to produce than chemical pills like statins. When they first launched, annual prices were over $14,000. Since then, manufacturers have cut prices and offered patient assistance programs. Still, even with discounts, they’re 3 to 5 times more expensive than statin-plus-ezetimibe combinations.
Can you stop taking statins if you start PCSK9 inhibitors?
It depends. Many patients take both together for maximum effect. In some cases, especially if statin side effects were the problem, doctors may reduce or stop the statin. But because statins have proven long-term benefits beyond just lowering LDL, many doctors prefer to keep them on board unless there’s a clear reason to stop.
Do PCSK9 inhibitors cause memory problems?
No clinical trials or large studies have linked PCSK9 inhibitors to memory loss or cognitive decline. Unlike statins, which some patients report affect their thinking, PCSK9 inhibitors have shown no negative impact on brain function in over 10 years of follow-up data.
Is there a cheaper alternative to PCSK9 inhibitors?
Yes. Ezetimibe (Zetia) is a pill that lowers LDL by about 15-20% and costs under $20 a month. Bempedoic acid (Nexletol) is another oral option that reduces LDL by 20-25% with fewer muscle side effects than statins. Both are often used before jumping to PCSK9 inhibitors. Inclisiran (Leqvio), a twice-yearly injection, is also becoming more available and may offer a middle ground in cost and convenience.
How long do you need to take PCSK9 inhibitors?
Like statins, PCSK9 inhibitors are meant for long-term use. Stopping them means your LDL will rise again - usually within weeks. Most patients stay on them indefinitely, especially if they have heart disease or inherited high cholesterol. Long-term studies show they remain safe and effective for at least five years, and likely longer.
When choosing between PCSK9 inhibitors and statins, there’s no perfect answer - only the best fit for your body, your life, and your goals. Talk to your doctor. Ask about your LDL numbers. Ask about your tolerance. Ask about cost. And remember: lowering cholesterol isn’t just about a number on a lab report. It’s about protecting your heart - for years to come.

Rachel Cericola
December 22, 2025 AT 06:06Let me break this down for anyone feeling overwhelmed - statins are the backbone of lipid management for a reason. Decades of RCTs, real-world data, and mortality reduction don’t lie. But PCSK9 inhibitors? They’re not magic. They’re precision tools for specific populations. If you’re a 65-year-old with ASCVD and LDL stuck at 110 on max rosuvastatin, yes - add evolocumab. If you’re a 40-year-old with borderline high cholesterol and mild statin intolerance? Try ezetimibe first. Or bempedoic acid. Or lifestyle. Don’t skip steps because the injectable looks fancy. Your insurance won’t cover it, your body doesn’t need it, and your wallet will thank you.
Also - muscle pain isn’t always statin-related. Many people confuse normal aging, vitamin D deficiency, or hypothyroidism with statin myopathy. Get your CK levels checked before quitting. And yes, the brain fog? Mostly placebo effect. Double-blind studies show no cognitive decline vs placebo. Stop blaming the pill. Start looking at sleep, stress, and screen time.
PCSK9 inhibitors? They’re a win for familial hypercholesterolemia patients. That 42-year-old woman with LDL 286? She’s the reason these drugs exist. But don’t let the hype make you think they’re for everyone. Medicine isn’t a grocery store. You don’t get to pick the most expensive item because it ‘sounds better.’
Christine Détraz
December 23, 2025 AT 22:49I switched from atorvastatin to alirocumab last year after six months of leg cramps that made walking to the fridge feel like a marathon. Honestly? Life changed. No more foggy mornings. No more wondering if my brain was melting. The injection? Annoying at first - I cried the first time. But now it’s like brushing my teeth. Refrigerator? Yeah, I keep it in the door so I don’t forget. And the cost? My insurer denied me twice. I wrote letters. Called my senator. Got approved on the third try. Worth every second. I’m not saying everyone needs this. But if you’re suffering and statins aren’t working? Don’t give up. Keep pushing. You’re not crazy. Your pain is real.
Also - the idea that we’re overprescribing these? No. We’re underprescribing them to the people who actually need them. The real scandal is the 80% of FH patients who never get diagnosed.
And yes - I still take a low-dose statin. My doc says it’s better together. So I do. Science > ego.
Blow Job
December 24, 2025 AT 19:52Man I used to hate needles. Like, full-on panic attacks. But after my heart attack and seeing my LDL stay at 140 on max Lipitor, I was like… fine. I’ll poke myself. Turns out the pen is like a fancy Bic. No pain. Just a tiny pinch. And now? My numbers are in the 30s. I feel like a new person. No more tired all the time. No more ‘am I losing my mind?’ moments.
Statins made me feel like a zombie. This? This feels like living.
Cost sucks. But I’d rather pay $300 a month than $300k for a stent next year. Just saying.
Ajay Sangani
December 25, 2025 AT 19:44It’s funny how we treat cholesterol like it’s the enemy. But cholesterol isn’t bad - it’s essential. It’s the building block of every cell membrane, of hormones, of vitamin D. The real issue isn’t cholesterol - it’s inflammation. It’s endothelial damage. It’s sugar, processed oils, chronic stress. Statins reduce inflammation too - that’s why they work. But we’ve turned a complex physiological imbalance into a simple pill problem. We’re treating symptoms, not causes.
PCSK9 inhibitors? They’re brilliant. They’re elegant. But they’re still a bandage on a bullet wound. We need systemic change - in food policy, in healthcare access, in how we define ‘health.’
Still… if I had to choose between a $10 pill and a $10k injection? I’d take the injection. Because sometimes, survival isn’t about philosophy. It’s about staying alive long enough to fix the system.
Pankaj Chaudhary IPS
December 26, 2025 AT 07:05As a physician who has treated over 300 patients with hyperlipidemia, I can confirm: statins remain the cornerstone. But let us not dismiss the dignity of those who cannot tolerate them. PCSK9 inhibitors are not a luxury - they are a necessity for those with familial hypercholesterolemia and established cardiovascular disease. In India, where access to generics is widespread, statins are a triumph of public health. But in the U.S., where insurance barriers exist, we are failing the very people we claim to protect.
Let us not confuse cost with value. A $14,000 drug that prevents one heart attack saves $250,000 in hospital costs. The math is clear. The moral imperative is clearer.
To those who say ‘just eat better’ - you have never seen a 45-year-old man with LDL 320 and no dietary vice. This is genetics. This is biology. This is not laziness.
Gray Dedoiko
December 28, 2025 AT 04:33Just wanted to say - I’m a 52-year-old guy who started statins after my first angioplasty. Lasted 4 months. Muscle pain so bad I couldn’t lift my coffee cup. Tried every generic. Same thing. My cardiologist suggested PCSK9. I thought I’d die from the needle. Turns out I’m fine. The only thing I miss? Not having to remember to refrigerate it. And yeah, I still feel weird about injecting myself. But I’d rather be alive and weird than dead and ‘normal.’
Also - the memory thing? I thought I was going crazy. Turns out I was just tired. Sleep helped more than any pill.
Aurora Daisy
December 29, 2025 AT 22:21Oh look, another article where the ‘experts’ pretend we’re all just rational actors with perfect access to healthcare. Let me guess - you’ve never waited 6 months for a prior auth. Never had your insurance deny a drug because you didn’t ‘fail’ a cheaper one first. Never had to cry because your kid’s dad needs a $12,000-a-year injection to not die.
Statins are great. For people who can afford them. For people who don’t have to choose between meds and rent. For people whose doctors actually listen.
Meanwhile, I’m over here reading about ‘clinical trials’ while my neighbor’s brother died of a heart attack because his insurance said ‘try ezetimibe first.’
It’s not a medical debate. It’s a moral failure dressed up as science.
John Pearce CP
December 31, 2025 AT 01:14Let me be blunt. The American healthcare system has turned a life-saving class of drugs into a status symbol for the wealthy. PCSK9 inhibitors are not ‘better’ - they are more expensive. And that’s the only difference. Statins have saved millions. They are the product of decades of rigorous, publicly funded research. Meanwhile, these injectables were developed by private firms who priced them at $14,000 to recoup R&D - even though the science was built on NIH-funded work.
This isn’t innovation. It’s exploitation. And the fact that doctors prescribe them without questioning the cost? That’s complicity.
If you can’t afford statins, you shouldn’t be alive in this country. And if you can afford PCSK9 inhibitors? You’re already part of the problem.
Jillian Angus
January 2, 2026 AT 00:45My mom’s on Repatha. She’s 71. Has had two stents. Can’t take statins. She hates the shots but does them anyway. She says it’s the only thing that lets her play with her grandkids without feeling like her legs are made of lead. I asked her if she’d rather take a pill. She said ‘I’d rather take a needle than a coffin.’
I don’t know what to say to that.
Cost? Yeah it’s insane. But I’d rather pay for a needle than a funeral.
Also - I cry every time I hear her say ‘I’m still here.’
niharika hardikar
January 3, 2026 AT 19:42It is imperative to underscore that the pharmacological intervention paradigm currently dominant in Western cardiology is predicated upon an overreliance on pharmacodynamic modulation at the expense of upstream determinants of cardiovascular risk. Statins, despite their pleiotropic effects, remain the most cost-effective intervention in the context of population-level health economics. PCSK9 inhibitors, while demonstrating statistically significant LDL-C reduction in randomized controlled trials, have not yet demonstrated sufficient incremental benefit in all-cause mortality to justify their incremental cost-effectiveness ratio in low-risk cohorts.
Furthermore, the phenomenon of ‘statin intolerance’ is frequently overdiagnosed. A 2023 meta-analysis in JAMA Cardiology demonstrated that 90% of patients reporting myalgia demonstrated no elevation in creatine kinase levels, suggesting a nocebo effect. The clinical imperative is to rechallenge with low-dose statins, co-administer coenzyme Q10, and optimize vitamin D status prior to escalation to biologics.
One must not conflate efficacy with accessibility. The moral hazard of permitting high-cost biologics to become de facto first-line therapy in affluent populations exacerbates global health inequity.
CHETAN MANDLECHA
January 5, 2026 AT 02:46Statins work. But I took them for 3 years. Felt like I was walking through wet cement. My legs hurt. My brain felt like it was wrapped in cotton. I stopped. My LDL went up. I didn’t care. I was tired of feeling sick just to live longer.
Then I found out about inclisiran. Two shots a year. No daily pills. No injections every two weeks. I got it last month. My LDL dropped 50%. I still feel like me.
It’s not perfect. But it’s the closest thing to a win I’ve had since my diagnosis.
Also - my doctor didn’t even mention it until I asked. Why?
Paula Villete
January 6, 2026 AT 00:49So I tried statins. Felt like my bones were made of glass. Tried PCSK9. Injected myself. Cried. Then laughed. Then cried again. My LDL went from 180 to 42. I can breathe. I can sleep. I can think.
But here’s the thing - I didn’t know any of this until I spent 3 months reading Reddit threads and patient forums. My doctor didn’t tell me about inclisiran. Didn’t mention bempedoic acid. Just said ‘take this pill.’
So I did. And I got sick.
Now I’m the one telling people: ask for the alternatives. Don’t accept ‘it’s the standard.’ Ask for the data. Ask for the cost. Ask for the hope.
And if you’re a doctor? Stop being a salesman. Be a guide.
EMMANUEL EMEKAOGBOR
January 7, 2026 AT 18:47In Nigeria, we don’t have PCSK9 inhibitors. We don’t even have good access to statins in rural areas. But we have diet. We have movement. We have community. My uncle had high cholesterol. He didn’t take pills. He walked to market every day. Ate yams, not fried plantain. Drank hibiscus tea. Lived to 89.
Maybe the real question isn’t which drug is better - but why we’ve forgotten how to live.
Still - if I could give my son a pill that stops him from dying before 50? I’d sell my goat for it.
Pankaj Chaudhary IPS
January 8, 2026 AT 11:57Thank you for sharing your experience, Christine. Your story echoes the lived reality of countless patients who are forced to become experts in their own care because the system fails them. This is not a pharmacological dilemma - it is a failure of medical paternalism. We must empower patients to demand alternatives, to question cost barriers, and to refuse to be passive recipients of care. The future of medicine lies not in the most expensive drug, but in the most dignified conversation between physician and patient. Keep speaking. Keep advocating. The system hears you.