Diabetes Medication Side Effect Selector
Find Your Best Diabetes Medication
Select your health profile and priorities to discover which medications match your needs based on side effect profiles.
Your Health Profile
Your Biggest Concern
When you’re first diagnosed with type 2 diabetes, the focus is often on lowering your blood sugar. But after a few weeks or months, you start noticing something else: the side effects. Nausea. Frequent bathroom trips. Dizziness. Weight gain. These aren’t just inconveniences-they can make you stop taking your medicine altogether. That’s why choosing diabetes medications based on side effect profiles isn’t just a good idea-it’s essential for long-term success.
Metformin: The Starting Point, But Not Without Hiccups
Most doctors still start with metformin. It’s cheap, effective, and doesn’t cause low blood sugar or weight gain. But about 30% of people get stomach issues-diarrhea, cramps, nausea-especially when they first start. The good news? These usually fade after a few weeks. If they don’t, switching to the extended-release version cuts those side effects in half. One study showed that 82% of users found the extended-release form much easier to tolerate. Start low: 500 mg once a day with dinner. Slowly bump it up by 500 mg every week. Most people reach the full 2,000 mg dose within a month without quitting.
Metformin is safe for kidneys-unless your eGFR drops below 30. Then it’s a no-go. But for most people, it’s the best first choice. It doesn’t make you gain weight. It doesn’t crash your blood sugar. And it’s been around since 1995 for a reason.
Sulfonylureas: Low Cost, High Risk
Drugs like glimepiride and glibenclamide have been used for decades. They work well to lower blood sugar. But they also cause low blood sugar-often without warning. Glibenclamide triggers hypoglycemia in 77% of users. Glimepiride? Still bad at 44%. That’s why doctors avoid them in older adults or anyone with irregular meals. If you’re 70, live alone, or drive for a living, this isn’t the drug for you.
They also make you gain weight. Glimepiride adds about 26% more body weight over time. Glibenclamide? Less, but still enough to undo other health gains. A Diabetes Strong survey found that 44% of people quit sulfonylureas within a year-mostly because of low blood sugar or weight gain. If you’re prescribed one, ask if glimepiride is an option over glibenclamide. It’s safer. Still, many end up switching to something else within months.
SGLT-2 Inhibitors: Blood Sugar Down, Infections Up
Empagliflozin and dapagliflozin are part of a newer class called SGLT-2 inhibitors. They don’t just lower blood sugar-they help your heart and kidneys. For people with heart failure or chronic kidney disease, these are now first-line options. But they come with a trade-off: yeast infections.
Women get genital yeast infections in about 8-11% of cases. Men? Around 1-4%. It’s not dangerous, but it’s annoying. Urinary tract infections happen in 4-8% of users. The fix? Good hygiene. Wipe front to back. Keep dry. Don’t sit in wet clothes. One clinic in Michigan cut infection-related discontinuations by 35% just by teaching patients simple hygiene steps.
There’s also a rare but serious risk: Fournier’s gangrene-a life-threatening infection of the genitals. It’s extremely rare (0.002%), but the FDA now requires warnings. Most people never see it. But if you notice sudden pain, swelling, or fever in that area, get help immediately.

GLP-1 Receptor Agonists: Nausea at First, Weight Loss Later
Liraglutide, semaglutide, and tirzepatide are injectables that mimic a gut hormone. They lower blood sugar, reduce appetite, and help you lose weight. In trials, tirzepatide led to over 15% body weight loss. That’s more than most diets. But the catch? Nausea.
Up to 45% of people feel sick when they start. Vomiting and diarrhea are common too. But here’s the secret: if you stick with it past 8 weeks, the nausea drops. In one study, people who waited got nausea down from 45% to 18% by going slow. Start at the lowest dose. Wait four weeks before increasing. Most people who push through end up loving the weight loss. One user on MyNetDiary lost 7.2 kg in six months and said the nausea was worth it.
These drugs are now recommended as first-line for people with obesity (BMI ≥30) or heart disease. They’re expensive, but their benefits are real. And with new generics coming, prices may drop soon.
DPP-4 Inhibitors: The Middle Ground
Drugs like sitagliptin and linagliptin are oral pills that don’t cause weight gain or low blood sugar-unless you combine them with sulfonylureas. Alone, they’re gentle. Hypoglycemia risk is only 2-5%. Side effects? Mostly mild: stuffy nose, headache, sore throat.
They’re ideal for older adults or people with kidney problems. Linagliptin doesn’t need a dose change even if your kidneys are weak. Saxagliptin does. That’s a big deal if you’re on dialysis or have stage 3 kidney disease. AACE guidelines specifically recommend DPP-4 inhibitors for kidney patients because they’re easier on the system.
One review of 1,245 sitagliptin users found 78% gave it 4 or 5 stars. The complaints? Joint pain and colds. But overall, it’s one of the most tolerated drugs out there.
Thiazolidinediones: Rarely Used for a Reason
Pioglitazone and rosiglitazone used to be popular. Now? Not so much. Rosiglitazone was banned in Europe because it raised heart attack risk. Pioglitazone? It’s still available, but it’s got its own red flags.
It increases the risk of bladder cancer by 27% after two years of use-especially at doses over 80 mg/day. It also causes fluid retention, which can worsen heart failure. And bone fractures? 50% more likely than with metformin. Most doctors won’t touch it unless someone has no other options. Even then, they monitor closely.
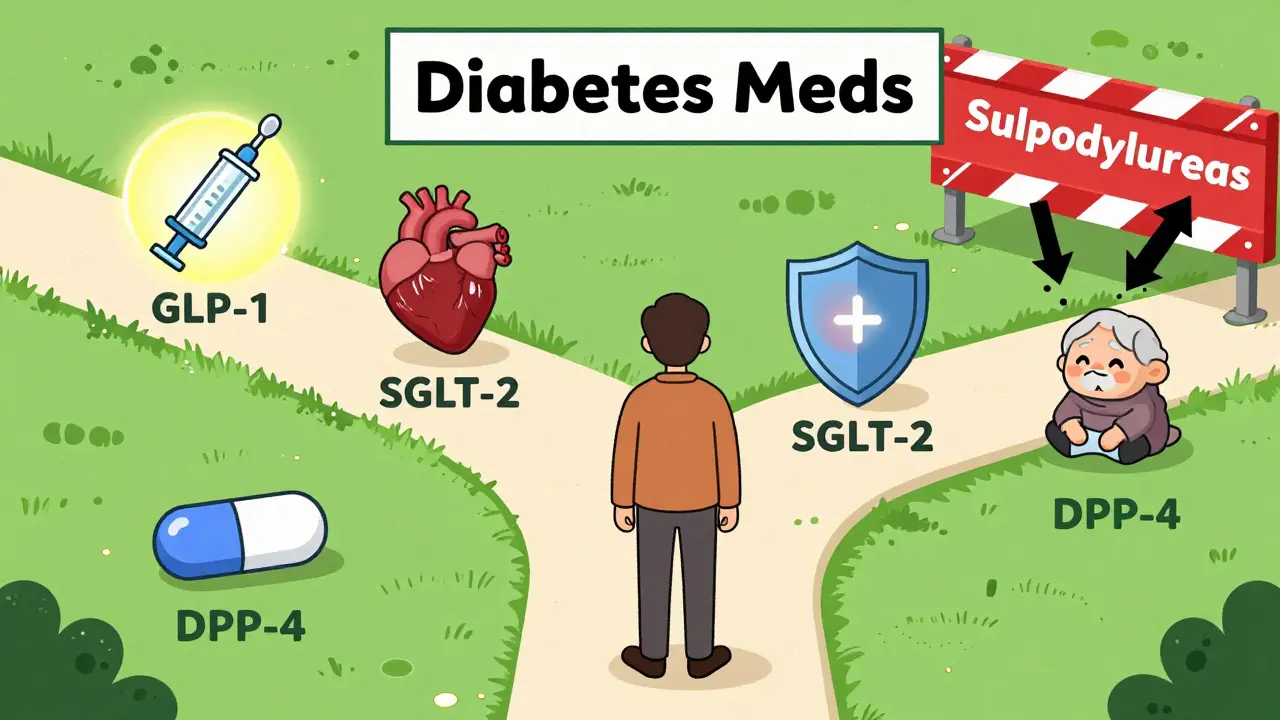
Putting It All Together: Your Side Effect Game Plan
There’s no one-size-fits-all. Your best drug depends on your life, your health, and what you can live with.
- If you’re young, healthy, and want to avoid weight gain? Start with metformin. Go slow. Use extended-release if GI issues hit.
- If you have heart disease or kidney disease? SGLT-2 inhibitors (empagliflozin, dapagliflozin) are now top choices. Manage infections with hygiene.
- If you’re overweight and want to lose weight? GLP-1 agonists (semaglutide, tirzepatide) are powerful. Push through the nausea-it gets better.
- If you’re older or have unpredictable meals? Skip sulfonylureas. Go for DPP-4 inhibitors or SGLT-2s instead.
- If you have kidney problems? Avoid metformin below eGFR 30. Use linagliptin. Avoid pioglitazone.
Side effects aren’t just annoying-they’re deal-breakers. If you quit your medicine because of nausea or yeast infections, your blood sugar climbs. Your risk of heart attack, stroke, or kidney failure goes up. That’s why choosing based on side effects isn’t optional. It’s survival.
What’s Next? The Future of Diabetes Meds
Doctors are already moving away from drugs that cause low blood sugar or weight gain. The market is shifting fast. In 2018, only 8.7% of new prescriptions were for GLP-1 drugs. By 2022, that jumped to 24.1%. By 2028, experts predict over half of all diabetes meds will be chosen for their weight loss and low hypoglycemia risk.
New drugs are coming. Tirzepatide (Mounjaro) already shows better weight loss than semaglutide. Smart insulins-ones that only activate when blood sugar is high-are in trials. Even microbiome treatments are being tested to reduce metformin’s stomach issues. One pilot study showed a probiotic cut diarrhea by 40%.
What matters now isn’t just whether a drug lowers A1C. It’s whether you can stick with it. And that starts with knowing your side effect limits.
Which diabetes medication has the fewest side effects?
DPP-4 inhibitors like linagliptin and sitagliptin generally have the mildest side effects. They rarely cause low blood sugar or weight gain. Common issues are mild: stuffy nose, headache, or sore throat. They’re a good choice for older adults or people with kidney disease who need something gentle.
Can metformin cause long-term damage?
No. Metformin doesn’t cause long-term organ damage. The only real risk is lactic acidosis, which is extremely rare-3 to 10 cases per 100,000 patient-years-and mostly happens in people with severe kidney failure (eGFR below 30). For most people, it’s one of the safest diabetes drugs ever made. GI side effects are temporary and manageable.
Why do some diabetes meds cause weight gain and others cause weight loss?
It’s about how they work. Sulfonylureas and insulin push your body to store more glucose as fat. GLP-1 agonists and SGLT-2 inhibitors do the opposite-they reduce appetite, slow digestion, and make your body burn more sugar through urine. That’s why one class makes you gain weight and the other helps you lose it.
Are SGLT-2 inhibitors safe for women?
Yes, but they can cause genital yeast infections in about 8-11% of women. These aren’t dangerous but can be uncomfortable. They’re easily treated with over-the-counter antifungals. Good hygiene-drying thoroughly after showers, avoiding tight clothing-cuts risk by up to 35%. The heart and kidney benefits often outweigh this side effect.
What should I do if I can’t tolerate my diabetes medication?
Don’t quit cold turkey. Call your doctor. There’s almost always another option. If metformin gives you stomach pain, try extended-release. If a GLP-1 agonist makes you nauseous, slow the dose increase. If you keep having infections with an SGLT-2 inhibitor, switch to a DPP-4 inhibitor. Your treatment plan should fit your life-not the other way around.
Final Thought: Your Body, Your Rules
Diabetes isn’t just about numbers on a screen. It’s about how you feel every day. If your medicine makes you sick, tired, or anxious, it’s not working-even if your A1C looks good. The best drug is the one you’ll take tomorrow, next month, and next year. That’s why side effect profiles matter more than ever. Talk to your doctor. Ask about alternatives. Be honest about what you can handle. Your health depends on it.

bhushan telavane
December 19, 2025 AT 05:02Metformin made me feel like a ghost in my own body for the first two weeks. Extended-release? Game changer. No more midnight bathroom marathons. Just quiet, steady control. I wish I’d known this sooner.
Connie Zehner
December 20, 2025 AT 00:44OMG I CRIED WHEN I GOT MY FIRST YEAST INFECTION FROM DAPAGLIFLOZIN 😭 I WAS LIKE ‘WHY IS MY LIFE LIKE THIS’ BUT THEN I LOST 18 LBS AND MY BP DROPPED SO NOW I’M LIKE… maybe it’s worth it? 🤷♀️😂
holly Sinclair
December 21, 2025 AT 06:55It’s fascinating how pharmacodynamics intersect with lived experience here. The biological mechanism of SGLT-2 inhibition-renal glucose excretion-creates an osmotic diuresis that alters vaginal microbiota pH, thereby predisposing to candidiasis. But what’s ethically more significant is that patients are rarely warned about the psychosocial burden of recurrent genital infections-they’re treated as trivial side effects, when in reality they’re intimate, isolating, and stigmatizing. We need to reframe ‘tolerability’ as a holistic construct, not just a clinical metric.
mark shortus
December 21, 2025 AT 11:13GLP-1s are the FUTURE. I was SO done with diabetes. Then I started semaglutide. First 6 weeks? I wanted to die. Nausea so bad I cried in the grocery store. But then… BAM. I lost 22 lbs. My pants fell off. My wife cried. My doctor high-fived me. NOW I’M A CONVERT. If you’re scared-DON’T QUIT. PUSH. IT. GETS. BETTER. 🙌
Emily P
December 21, 2025 AT 22:08Is there data on how many people quit metformin because of GI issues but never tell their doctor? I think it’s way higher than reported.
Vicki Belcher
December 23, 2025 AT 01:22YOU GOT THIS 💪 Seriously-side effects suck, but you’re not alone. I started on sulfonylureas and almost gave up. Then switched to linagliptin and now I feel like myself again. Don’t settle. Ask for options. You deserve to feel good while managing this. ❤️
Jedidiah Massey
December 23, 2025 AT 08:39Metformin’s efficacy is predicated on AMPK activation and mitochondrial complex I inhibition-mechanisms that, while well-characterized, are often misattributed to ‘just lowering glucose.’ The real advantage lies in its pleiotropic effects on hepatic gluconeogenesis and insulin sensitivity. That said, the GI side effect profile remains a clinically significant barrier to adherence, particularly in populations with low health literacy. SGLT-2 inhibitors, meanwhile, demonstrate superior cardiovascular mortality reduction in HFrEF-per EMPA-REG OUTCOME. Yet, their cost-benefit ratio is skewed by institutional formularies. We’re not treating patients. We’re optimizing algorithms.
Lynsey Tyson
December 24, 2025 AT 16:44I just wanted to say thank you for writing this. I’ve been on 5 different meds over 8 years. I felt so alone. Reading this made me feel seen. I’m trying the extended-release metformin next week. Fingers crossed.
Sarah McQuillan
December 25, 2025 AT 23:43Actually, in India, metformin is the only thing they give you because it’s cheap. No one tells you about the extended-release version. You just suffer. And then they blame you for not ‘complying.’
Kitt Eliz
December 27, 2025 AT 22:24STOP QUITTING. I’m a nurse and I’ve seen this 100x. GLP-1 nausea peaks at week 3-then drops like a rock. Dapagliflozin infections? Wipe front to back. Wear cotton. No douches. Done. You’re not broken. Your med just needs tweaking. You got this. 💪🩺🔥
anthony funes gomez
December 28, 2025 AT 18:46Metformin doesn’t cause lactic acidosis unless eGFR<30, yes-but what about subclinical mitochondrial dysfunction? What about the gut microbiome disruption that precedes GI symptoms? The literature is silent on long-term epigenetic modulation. We’re treating symptoms, not systems. And we call this medicine?
Alana Koerts
December 30, 2025 AT 10:10This article is just a drug company ad with footnotes. Everyone knows SGLT-2 inhibitors increase DKA risk in type 2. No one talks about that. And GLP-1s cost $1000/month. You’re telling people to ‘push through’ nausea when they can’t even afford the pill? This is toxic.
Dikshita Mehta
December 31, 2025 AT 07:43My mom in Delhi started on metformin ER and now she’s biking 5km every morning. No more dizziness. No more bloating. She says the key was starting at 500mg and waiting. Don’t rush it. Small steps. Big results. 🙏