Sodium Balance: How to Spot Problems and Fix Them
Ever feel dizzy after a workout or notice sudden confusion in an older relative? Sodium — the salt in your body — plays a big role in blood pressure, nerves, and fluid balance. Too little or too much can cause clear problems. Here’s a straightforward guide to what causes sodium imbalance, how to recognize it, and practical steps you can take right away.
Common causes and symptoms
Low sodium (hyponatremia) happens when blood sodium drops below 135 mmol/L. That can come from drinking too much water, certain diuretics, heart failure, kidney issues, or hormonal problems like SIADH. Symptoms include nausea, headache, tiredness, muscle cramps, confusion, and in serious cases seizures.
High sodium (hypernatremia) is when levels rise above 145 mmol/L. It usually means the body lost water faster than sodium — from fever, sweating, diarrhea, or not drinking enough. Symptoms include extreme thirst, dry mouth, restlessness, muscle twitching, and confusion. Severe cases can lead to coma.
Practical fixes you can try today
First, check your fluids. If you’re sweating a lot during exercise or hot weather, replace salts and fluids with an electrolyte drink or a homemade mix: clean water with a pinch of salt and a squeeze of citrus. For long workouts, choose sports drinks with sodium rather than plain water to avoid diluting blood sodium.
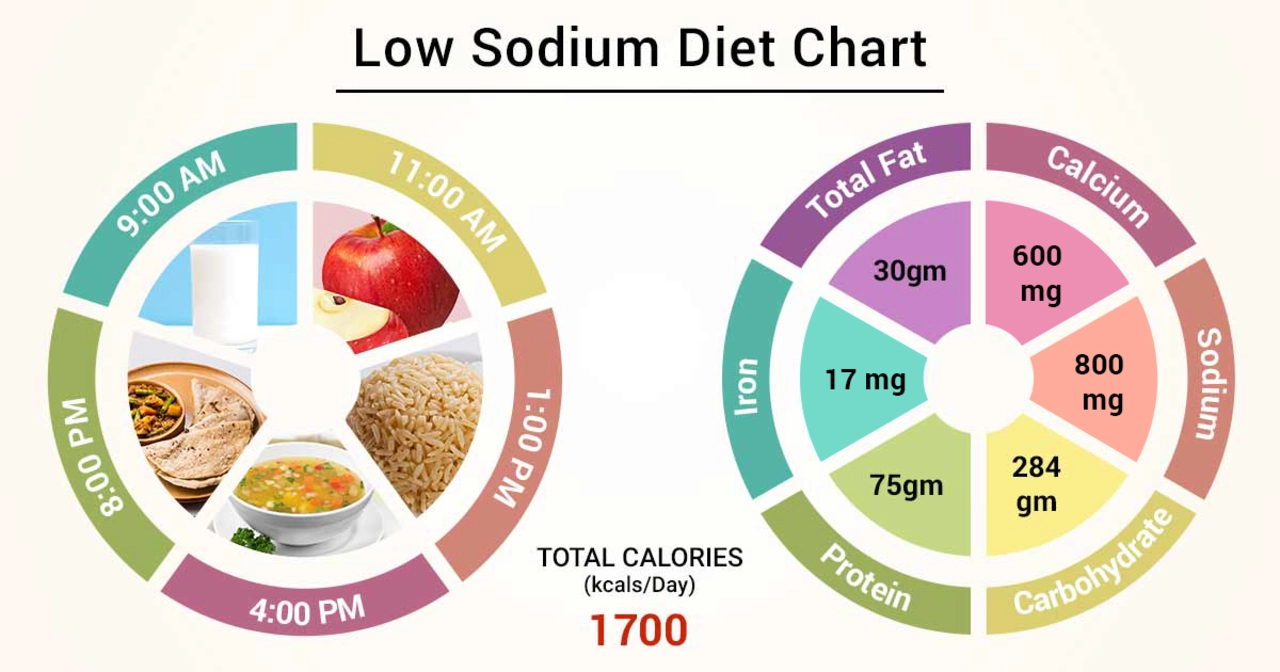
Look at your diet. Most people eat too much processed food, which raises sodium. Aim for under 2,300 mg daily, or 1,500 mg if your doctor tells you so. Read nutrition labels, cut back on canned soups, deli meats, and packaged snacks, and use herbs and lemon for flavor instead of salt.
Watch medicines. Diuretics, some antidepressants, and pain medicines can shift sodium. If you start feeling weak, confused, or unusually thirsty after a new drug, call your provider. Do not stop prescribed meds without medical advice.
When to test. Ask for a basic metabolic panel if you have unexplained dizziness, confusion, swelling, or sudden weight changes. Blood sodium is an easy test and it guides immediate care. For persistent or severe symptoms, go to the ER — seizures, fainting, or loss of consciousness are emergencies.
Adjust slowly. Treating sodium problems too fast can be dangerous. Medical teams correct levels at a controlled pace using IV fluids or medications like aldactone in specific cases. That’s why guided care matters.
Small daily habits help: drink when thirsty, eat whole foods, check labels, and mention any faintness or confusion to your doctor. Sodium balance affects energy, thinking, and heart health — a few practical moves can make a big difference.
If you have chronic conditions like heart failure, liver disease, or kidney problems, your sodium target may be lower and your doctor might check levels more often. Older adults and infants need careful fluid balance. Keep a simple log: write what you drink, salt added, symptoms, and weight changes. Bring that to appointments. Small records help doctors spot trends and adjust treatment faster. Ask questions every visit.
The Role of Diet in Preventing and Managing Hyponatremia
- by Colin Edward Egan
- on 15 May 2023
In my latest blog post, I discussed the role of diet in preventing and managing hyponatremia, a condition characterized by low sodium levels in the blood. I emphasized the importance of maintaining a balanced diet, which includes consuming adequate amounts of sodium to help regulate fluid balance in the body. In addition, I explored how drinking enough water, avoiding excessive consumption of sodium-rich foods, and being mindful of medications can help prevent and manage this condition. By paying attention to our diet, we can greatly reduce our risk of developing hyponatremia and lead a healthier life. Stay tuned for more tips on maintaining a balanced diet and overall well-being!
