Heparin Sodium: Uses, Dosage, Risks, and Safe Handling
Heparin sodium is a fast-acting blood thinner doctors use to stop clots from forming or growing. It’s given by injection — either into a vein in the hospital or under the skin for short-term prevention. People get it when doctors suspect a deep vein thrombosis, during dialysis, after some surgeries, or when heart attacks and unstable angina need quick anticoagulation.
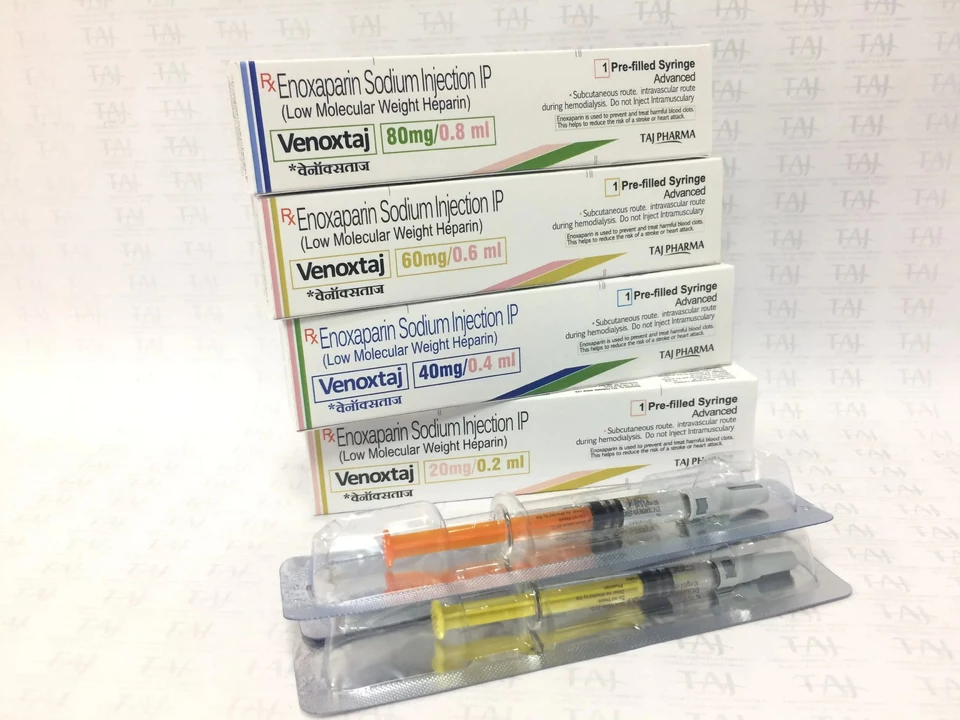
There are two common forms: unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) like enoxaparin. UFH is usually IV with dosing adjusted by lab tests. LMWH is given by fixed subcutaneous shots and is easier to use outside the hospital. Both reduce clotting but behave differently in the body and need different monitoring.
Quick dosing rules
Exact doses vary by reason for use, weight, and kidney function. For UFH a typical IV start might be a bolus followed by a continuous infusion adjusted to aPTT lab results. For LMWH, common prophylaxis doses are a fixed daily or twice-daily injection based on weight; treatment doses are higher and weight-based. Never guess doses — they’re individualized and usually set by a clinician.
Watch for these warning signs
Bleeding is the most common risk. Look for unusual bruising, blood in urine or stool, nosebleeds, or heavy menstrual bleeding. Also watch platelet counts — heparin can cause heparin-induced thrombocytopenia (HIT), a drop in platelets that can paradoxically raise clot risk. If platelets fall or you notice severe skin reactions, call your provider immediately.
If bleeding becomes dangerous, clinicians use protamine sulfate to partially or fully reverse heparin’s effect. Reversal dosing depends on how much heparin was given and when.
Interactions matter. Combining heparin with antiplatelet drugs (aspirin, clopidogrel), NSAIDs, or other anticoagulants raises bleeding risk. Adjustments are common for people with kidney problems, the elderly, and those having surgery.
Handling and storage are simple but important: use sterile technique, keep injections sealed until use, and dispose of needles in a sharps container. Don’t reuse needles or share vials. Heparin for injections should come from a licensed pharmacy or a hospital; injectable anticoagulants bought from unreliable online sources can be fake or contaminated and are dangerous.
Monitoring includes regular aPTT or anti-Xa tests and frequent platelet counts while on heparin. Labs tell your team if doses need change. Tell your provider about all medicines, vitamins, and herbal supplements — even over-the-counter pain relievers — because they can raise bleeding risk. When long-term anticoagulation is needed, doctors switch to oral drugs like warfarin or DOACs, but heparin stays useful in pregnancy and hospital situations.
Pregnancy is a special case—heparin doesn’t cross the placenta, so UFH or LMWH is often preferred to many oral anticoagulants during pregnancy when anticoagulation is needed. Still, dosing and monitoring need close follow-up.
If you or a family member are starting heparin, ask these practical questions: Why is it needed now? How will dosing be checked? What are clear bleeding signs to watch for? Who should you call after hours? Clear answers make use safer and less stressful.
Heparin sodium storage and handling: Best practices for healthcare providers
- by Colin Edward Egan
- on 6 May 2023
As a healthcare provider, it's crucial to understand the best practices for handling and storing Heparin Sodium. First and foremost, always store it at room temperature, away from direct sunlight and moisture. Additionally, make sure to check the expiration date before use, and properly dispose of any expired medication. When administering Heparin Sodium, adhere to strict aseptic techniques to prevent contamination. Lastly, educate yourself and your staff on the possible side effects and interactions, ensuring patient safety and optimal treatment outcomes.
