Clinical Trials: How They Work, Read Results & Stay Safe
Want to know how medicines really get approved? Clinical trials are where researchers test whether a drug works and is safe for people. I’ll explain the phases, show you how to read results without feeling lost, and give simple rules to spot bad claims—so you can make smarter health choices and avoid scams.
Phase 1 tests safety and dose in a small group. Phase 2 looks for early signs the drug works. Phase 3 compares the drug to standard care in large groups to confirm benefit and monitor side effects. After approval, Phase 4 keeps watching for rare or late problems. Knowing the phase tells you how much we really know about a treatment.
How to read trial results
Start with size and outcomes: how many people were in each group and what the main result was. Look for absolute numbers, not only percentages. A 50% relative improvement may mean 2 out of 100 improved versus 1 out of 100. Check how long the study followed people—short follow-up can miss long-term harms. Read the side effect table and focus on serious events, not only minor symptoms.
Check who was included. Trials often skip older adults, pregnant people, or those with other illnesses. That affects whether results apply to you. Also note funding and conflicts of interest; industry-funded trials are common, and transparency matters. Finally, find the full paper or registry entry—press releases can exaggerate benefits.
Joining a trial and staying safe
If you consider joining, ask for the informed consent form and read it carefully. It should explain risks, benefits, who covers medical care, and what happens if something goes wrong. Ask how side effects are handled and whether you can withdraw without penalty. Talk with your regular doctor before enrolling.
Be wary of sites that promise guaranteed cures or sell “trial-only” drugs without published data. Legitimate trials register on public databases and publish results in peer-reviewed journals. Use resources like clinicaltrials.gov, university hospital listings, or trusted patient groups to find trials. Our site also covers related topics—like telehealth bundles, online pharmacy safety, and post-marketing checks—to help you navigate care beyond the trial.
Reporting problems helps everyone. If you have unexpected side effects, tell the trial team and report to your country’s regulator. That data feeds safety checks and can change how drugs are used. Quick tip: keep copies of all trial paperwork and a short daily symptom log to share with clinicians.
Quick checklist before you trust a trial claim: registered trial ID, published data, reasonable sample size, clear primary outcome, and transparent funding. If any of these are missing, ask questions. Understanding trials helps you spot real progress, avoid hype, and make safer choices about new drugs and where to buy them.
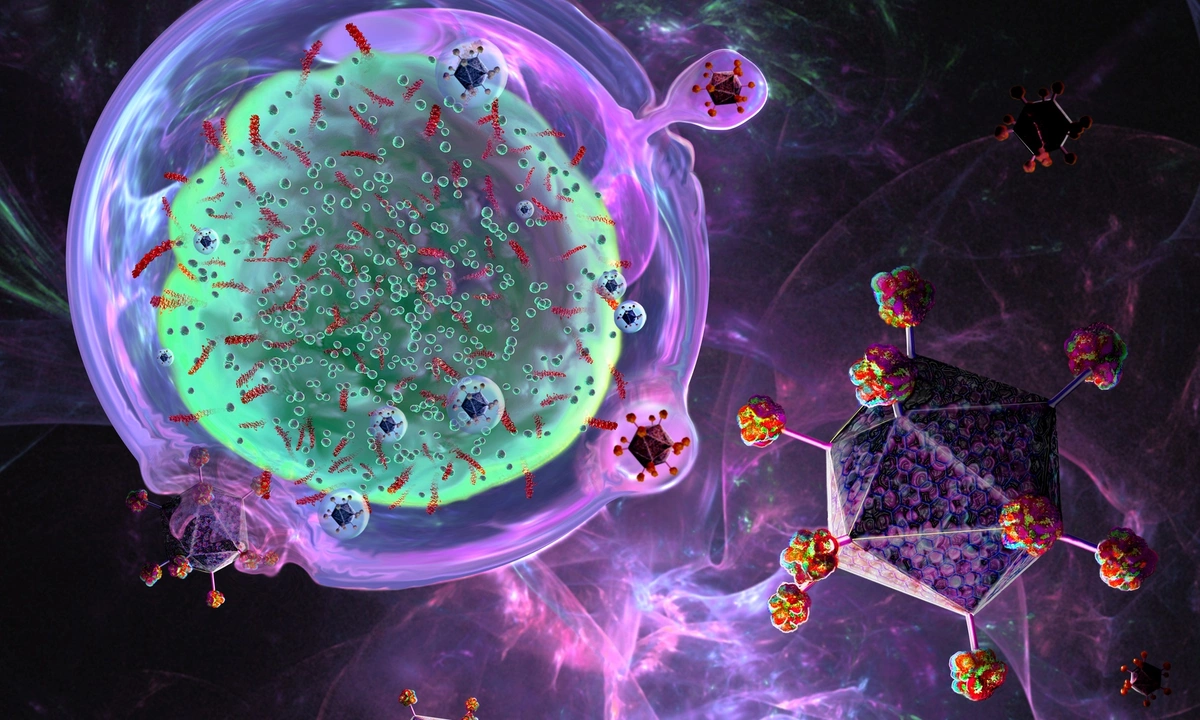
An Overview of Cell Lymphoma Clinical Trials
- by Colin Edward Egan
- on 27 May 2023
As a blogger, I have come across a plethora of information on cell lymphoma clinical trials. These trials are crucial in the development of new treatments and therapies for lymphoma, a type of cancer that affects the lymphatic system. Throughout my research, I discovered that clinical trials are typically divided into phases, each focusing on different aspects such as safety, dosage, and effectiveness. Patient participation is essential in these trials, as their experiences can lead to breakthroughs in the field. Overall, cell lymphoma clinical trials play a pivotal role in advancing our understanding and treatment of this complex disease.
