Atrial Tachycardia: What It Is and How It Affects You
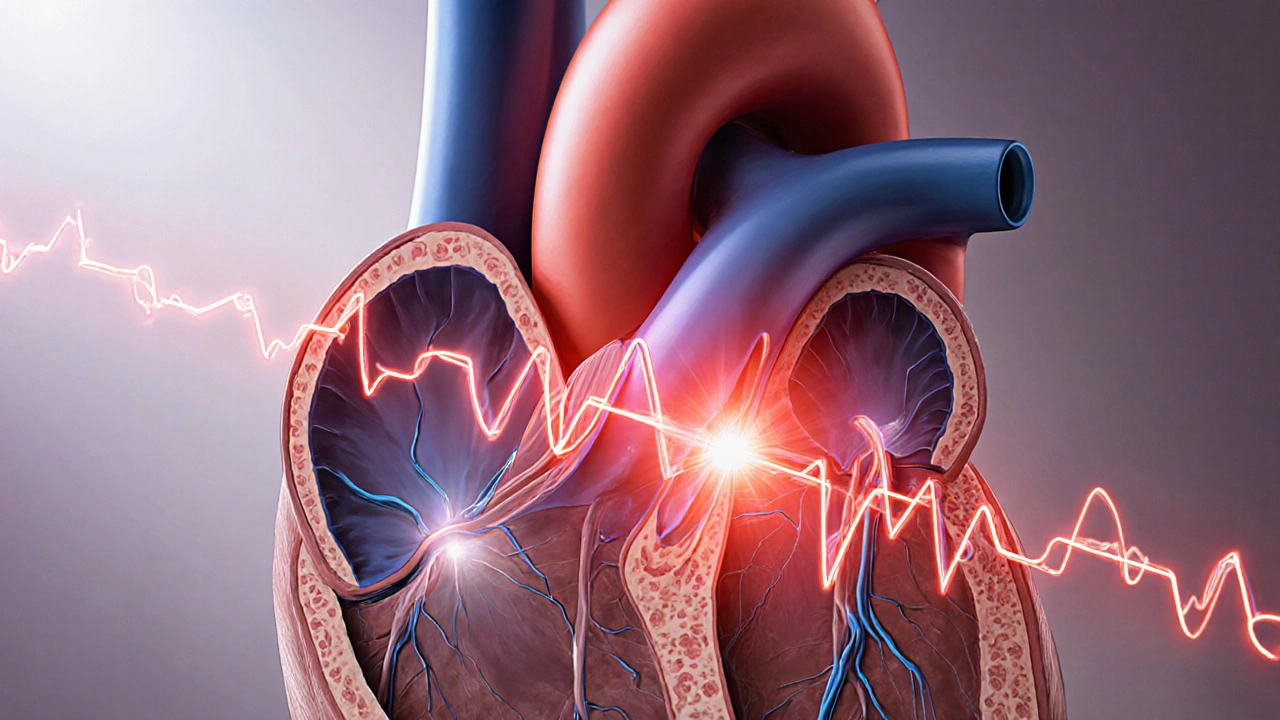
When working with atrial tachycardia, a rapid heart rhythm that originates in the atria. Also known as AT, it is a specific form of supraventricular tachycardia, the broader class of fast rhythms that start above the ventricles. Doctors often link it to other cardiac arrhythmias because the same electrical pathways are involved. Understanding these connections helps you see why a simple medication change or a more advanced test can make a big difference.
Atrial tachycardia typically shows up as a sudden fluttering in the chest, shortness of breath, or a feeling of “racing” when you’re at rest. The episodes can last seconds or stretch into hours, and the heart rate usually climbs above 100 beats per minute. One key reason it happens is an abnormal automatic focus in the atrial tissue that fires faster than the sinus node. This misfiring is often triggered by stress, caffeine, or underlying heart disease. When the focus is persistent, the heart’s timing gets thrown off, which can lead to fatigue and occasionally dizziness.
How Doctors Diagnose and Manage the Rhythm
First‑line treatment often involves beta blockers. These drugs slow the heart by blocking adrenaline’s effect on the SA node, which can blunt or stop an AT episode. In many cases, a low dose is enough to keep the rhythm in check without causing excessive fatigue. If beta blockers aren’t effective or cause side effects, doctors may turn to calcium‑channel blockers or anti‑arrhythmic pills like flecainide.
When medication doesn’t solve the problem, an electrophysiology study (EP study) comes into play. During this test, a specialist threads catheters into the heart to map the exact spot where the rapid signals start. The EP study not only confirms the diagnosis but also often doubles as a treatment session, because the physician can perform a catheter ablation to destroy the rogue tissue. Success rates for ablation of atrial tachycardia are high, especially when the origin is well‑localized.
Lifestyle tweaks can also tip the scales. Reducing caffeine, quitting smoking, and managing stress through meditation or regular exercise can lower the frequency of episodes. For athletes, the “training heart” can sometimes mask an AT, so a routine check‑up with a sports cardiologist is smart. If you have other heart conditions—like atrial fibrillation—keeping those under control is crucial because one arrhythmia often fuels the other.
It’s worth noting that atrial tachycardia isn’t just a nuisance; if left unchecked, it can weaken the heart muscle over time, leading to tachycardia‑induced cardiomyopathy. That’s why early detection and proper management matter. Blood tests, echocardiograms, and sometimes Holter monitors are used to assess the heart’s overall health and catch any hidden damage.
Below you’ll find a curated list of articles that dive deeper into each of these aspects—whether you’re looking for medication comparisons, step‑by‑step guides on buying generic heart drugs online, or the latest research on how specific therapies improve outcomes for atrial tachycardia patients. Use this resource to sharpen your understanding and take concrete steps toward better heart health.
Supraventricular Tachycardia Types Explained: AVNRT, AVRT, Atrial Tachycardia & More
- by Colin Edward Egan
- on 14 Oct 2025
Learn the key SVT types-AVNRT, AVRT, atrial tachycardia, and more-how they differ, how they're diagnosed, and the best treatment options.
