SVT Type Identifier Tool
SVT Type Identifier
Select your symptoms and ECG findings to determine which supraventricular tachycardia type might be most likely.
Likely SVT Type
When your heart suddenly rockets, you’ve likely experienced supraventricular tachycardia. Supraventricular Tachycardia is a fast heart rhythm that starts above the ventricles, usually between 150 and 250 beats per minute. It’s not a disease itself but a symptom of abnormal electrical pathways in the heart. Understanding the different sub‑types helps you recognize triggers, know what to expect from a doctor, and choose the right treatment.
Key Takeaways
- SVT covers several distinct rhythm disorders, each with its own trigger and treatment.
- AVNRT and AVRT are the two most common types, accounting for about 80% of episodes.
- Diagnosis relies on an electrocardiogram (ECG) and sometimes an electrophysiology study.
- Acute management can be as simple as a Valsalva maneuver, while chronic control may involve medication or catheter ablation.
- Lifestyle tweaks-stress control, caffeine reduction, adequate sleep-can cut down episodes for many patients.
What Is Supraventricular Tachycardia?
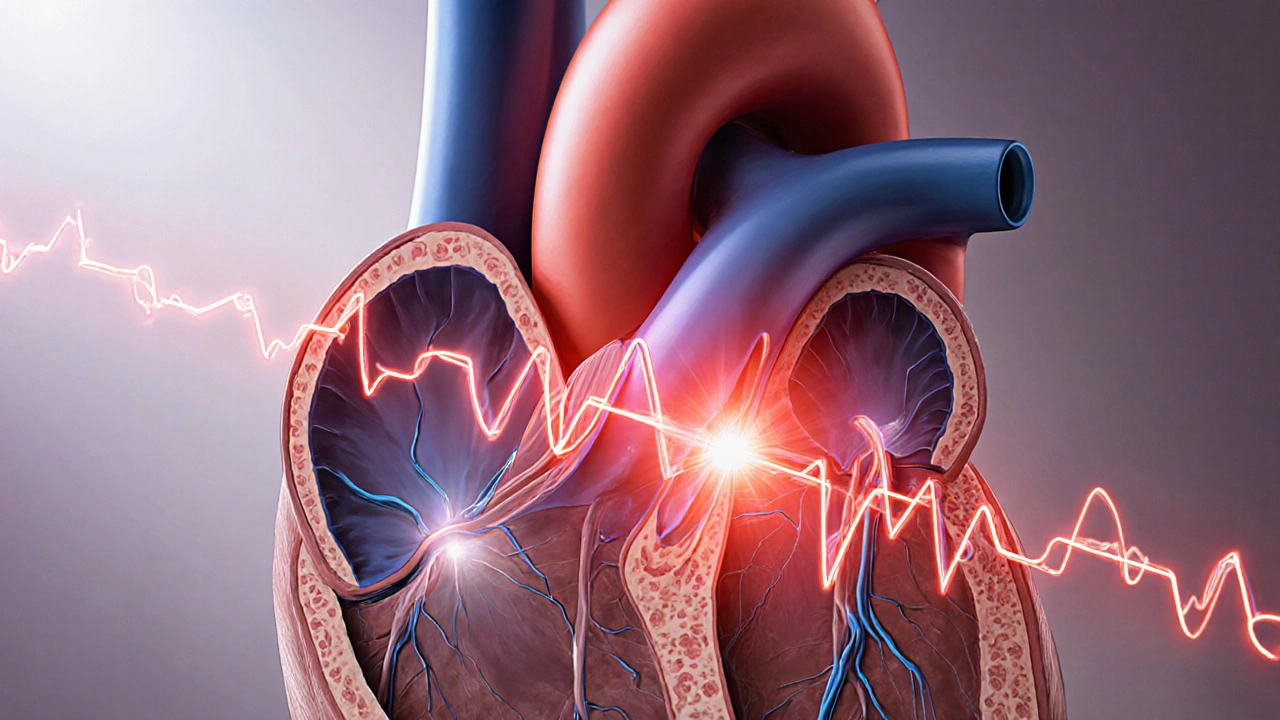
SVT is a blanket term for any rapid heartbeat that originates in the atria or the atrioventricular (AV) node, rather than the ventricles. The heart’s normal pace sits between 60 and 100 beats per minute. When an SVT episode kicks in, the rate jumps, often making you feel light‑headed, palpitations, chest discomfort, or shortness of breath.
Clinically, SVT is classified by the pathway that creates the fast rhythm. Understanding those pathways is key to proper treatment.
Main Types of SVT
Below are the six most commonly encountered SVT sub‑types. They differ in where the electrical circuit loops and how they respond to maneuvers or medication.
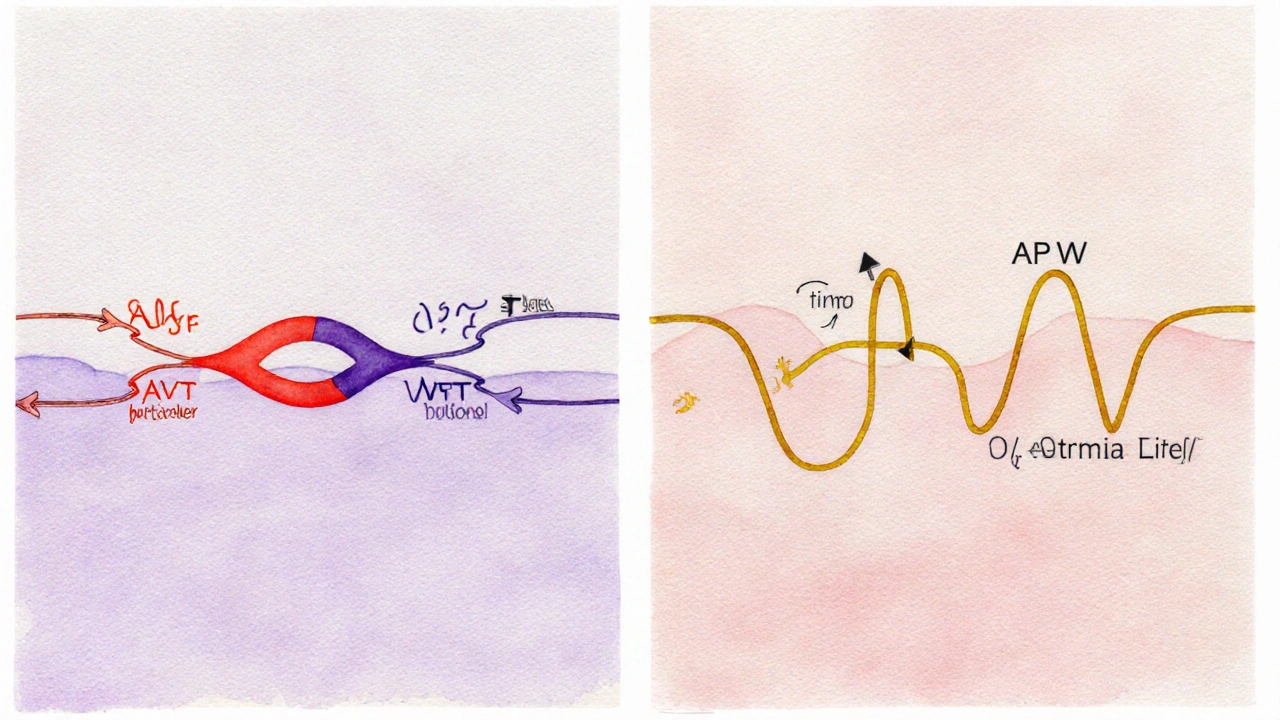
1. Atrioventricular Nodal Re‑entry Tachycardia (AVNRT)
AVNRT is the heavyweight champion of SVT, responsible for roughly 60% of cases. It uses two pathways within the AV node-a fast pathway that conducts quickly but recovers slowly, and a slow pathway that conducts slowly but recovers fast. When a premature heartbeat hits, the fast lane pauses while the slow lane keeps going, creating a re‑entry loop.
Typical ECG shows a narrow QRS complex and a short RP interval. Vagal maneuvers like the Valsalva often terminate the episode.
2. Atrioventricular Re‑entry Tachycardia (AVRT)
AVRT relies on an accessory pathway that bypasses the AV node. The most famous form is linked to Wolff‑Parkinson‑White Syndrome (WPW). In WPW, an extra bundle (the Bundle of Kent) lets impulses travel from the atria to the ventricles instantly, and then back up the AV node, forming a circuit.
ECG shows a short PR interval and a delta wave-those slurred up‑strokes on the QRS.
3. Atrial Tachycardia (AT)
Atrial Tachycardia originates from a single ectopic focus in the atria, not from the AV node. It’s less common but can be persistent. The heart rate often sits around 150‑200 bpm, and the ECG reveals P‑waves that look abnormal or occur earlier than expected.
4. Multifocal Atrial Tachycardia (MAT)
MAT features at least three different P‑wave morphologies, indicating several ectopic atrial foci firing. It’s usually seen in older patients with lung disease or electrolyte imbalances.
5. Orthodromic AVRT (Typical WPW)
When the impulse travels down the normal AV node and returns via the accessory pathway, the circuit is called orthodromic AVRT. The QRS stays narrow, making it look like AVNRT, but the presence of a delta wave on a baseline ECG clues you in.
6. Antidromic AVRT (Rare WPW Variant)
In antidromic AVRT, the impulse goes down the accessory pathway and back up through the AV node, producing a wide QRS complex that can mimic ventricular tachycardia.
How Doctors Diagnose SVT
Diagnosis starts with a careful history: onset, triggers, duration, associated symptoms. Physical exam may reveal a rapid pulse that can be felt at the wrist.
Key tools include:
- Electrocardiogram (ECG): Captures the rhythm, QRS width, PR interval, and any delta waves.
- Holter monitor or event recorder: Records heart rhythm over 24‑48hours or longer, catching intermittent episodes.
- Electrophysiology (EP) study: An invasive test where catheters map electrical pathways, pinpointing the exact SVT type.
Blood tests may be ordered to rule out thyroid disease, electrolyte disturbances, or drug effects that could provoke SVT.
Management and Treatment Options
Therapy follows a stepped approach-first try simple maneuvers, then medication, and finally procedural options if episodes are frequent or dangerous.
Acute Termination
- Vagal maneuvers: Valsalva, carotid sinus massage (only by a professional), or a cold‑water facial immersion.
- Rapid‑acting adenosine: A short IV push that briefly blocks AV node conduction, stopping AVNRT and orthodromic AVRT.
Long‑Term Control
- Beta‑blockers (e.g., metoprolol) - slow AV node conduction.
- Calcium‑channel blockers (e.g., diltiazem) - similar effect, useful if asthma limits beta‑blockers.
- Anti‑arrhythmic drugs such as flecainide or propafenone - especially for WPW patients without structural heart disease.
Catheter Ablation
Catheter ablation is a minimally invasive procedure that destroys the tissue responsible for the re‑entry circuit. For AVNRT, success rates exceed 95% with a low complication risk. WPW ablation targets the accessory pathway and can cure the condition permanently.
Recovery is quick-most patients return to normal activities within a week.
When to Seek Emergency Care
- Chest pain, fainting, or severe shortness of breath.
- SVT lasting longer than 24hours.
- History of heart disease or a known WPW pattern.

Living With SVT: Tips and Lifestyle
Even without medication, many people keep episodes at bay by tweaking daily habits.
- Limit caffeine and energy drinks-these can lower the threshold for triggers.
- Stay hydrated; dehydration can provoke arrhythmias.
- Practice stress‑reduction techniques-deep breathing, yoga, or meditation.
- Maintain a regular sleep schedule; sleep deprivation raises sympathetic tone.
- Track episodes with a smartwatch or app to identify personal triggers.
Regular follow‑ups with a cardiologist or electrophysiologist ensure that any change in pattern is evaluated promptly.
Comparison of Common SVT Types
| Type | Mechanism | Typical Rate (bpm) | ECG Hallmark | First‑line Treatment |
|---|---|---|---|---|
| AVNRT | Re‑entry within AV node (fast & slow pathways) | 150‑250 | Narrow QRS, short RP interval | Vagal maneuver → Adenosine |
| AVRT (WPW) | Accessary pathway (Bundle of Kent) creates loop | 150‑250 | Delta wave, short PR | Adenosine (orthodromic) / Ablation |
| Atrial Tachycardia | Single ectopic atrial focus | 130‑200 | Abnormal P‑wave morphology | Beta‑blocker or calcium‑channel blocker |
| Multifocal Atrial Tachycardia | Multiple atrial ectopic foci | 100‑130 (irregular) | ≥3 P‑wave shapes | Treat underlying lung disease, magnesium |
Frequently Asked Questions
Can SVT be life‑threatening?
Most SVT episodes are benign, but they can become dangerous if they last a long time, cause low blood pressure, or occur in people with structural heart disease. If you feel chest pain, faint, or shortness of breath, seek emergency care.
Why does adenosine stop an SVT?
Adenosine briefly blocks conduction through the AV node. Since most SVT circuits depend on the AV node, this interruption halts the re‑entry loop and restores normal rhythm within seconds.
Is catheter ablation safe?
Modern ablation uses sophisticated mapping and has a success rate above 95% for AVNRT and >90% for WPW. Complication rates are below 2%, typically minor vascular issues or transient heart block that can be managed with a pacemaker if needed.
Can lifestyle changes replace medication?
For many with infrequent episodes, reducing caffeine, managing stress, and staying hydrated can dramatically cut attacks. However, if episodes are frequent or symptomatic, medication or ablation remains the most reliable option.
What’s the difference between AVRT and WPW?
WPW is a specific form of AVRT caused by the Bundle of Kent accessory pathway, visible on a resting ECG as a delta wave. Not all AVRT patients have WPW; some have concealed pathways that only show up during an episode.

Terry Duke
October 14, 2025 AT 17:18Wow, this tool looks pretty slick, huh, it’s like having a mini‑cardiology clerk right in your browser, and the layout is clean, the options are clear, and it even throws a friendly reminder about seeing a cardiologist-nice touch!
For anyone who’s never dealt with SVT, this could demystify the jargon a bit, helping you spot patterns before you panic.
Just remember, it’s a guide, not a diagnosis, so keep your doctor in the loop.
Overall, kudos to the devs for making a complex topic feel approachable.
Stay curious, stay safe!
Chester Bennett
October 18, 2025 AT 21:18From a clinical perspective, the inclusion of both symptom checkboxes and ECG markers is essential, because SVT subtypes often overlap in presentation.
The heart‑rate range validation (60‑250 bpm) aligns well with typical tachyarrhythmia thresholds, preventing unrealistic inputs.
One suggestion: adding a brief description of the delta wave could help novices differentiate AVRT from other forms.
Overall the interface feels intuitive, and the disclaimer appropriately cautions users.
Good job on balancing detail with usability.
Samantha Leong
October 23, 2025 AT 01:18I totally get how scary it can be when your heart decides to race for no apparent reason.
What this tool does well is give you a concrete way to talk to your doctor-showing them the specific criteria you’ve selected.
It also reinforces that lifestyle tweaks-like limiting caffeine or managing stress-can sometimes reduce episode frequency.
Just keep a log of your episodes; that data combined with this tool can make your appointments much more productive.
Take care of yourself, and don’t hesitate to seek professional advice.
anshu vijaywergiya
October 27, 2025 AT 04:18The heart, that relentless drumbeat of life, can suddenly betray us with a wild, unbidden tachycardia that feels like a storm raging within our chest.
When you stare at the baffling squiggles on an ECG, the fear can be palpable, as if the lines themselves are whispering secrets you cannot decode.
This SVT Type Identifier steps onto the stage like a seasoned maestro, guiding the audience through a labyrinth of symptoms and waveforms.
By selecting the pulse of your heart-a rate that climbs beyond the ordinary-you already set the first clue on the investigative board.
The inclusion of chest pain, shortness of breath, and light‑headedness captures the triad of distress that patients frequently voice.
Moreover, the ECG findings-delta wave, abnormal P‑wave morphology, multiple P‑wave shapes, short RP interval-are not mere technical jargon but the fingerprints of distinct arrhythmic villains.
For instance, a delta wave screams accessory pathway involvement, pointing toward AVRT or the classic WPW syndrome.
Conversely, a short RP interval may hint at AVNRT, the most common form of SVT that often masquerades as palpitations.
The tool’s logical flow mirrors the diagnostic reasoning taught in the halls of electrophysiology, yet it is packaged in a friendly, web‑based format.
As a result, patients who once felt powerless can now articulate their experience in medically accurate language.
This empowerment can transform a clinical encounter from a monologue into a collaborative dialogue.
However, the tool wisely warns that it does not replace a cardiologist’s expertise, preserving the essential boundary between self‑education and professional care.
In practice, combining the output of this identifier with a thorough history and a physical exam yields a powerful diagnostic synergy.
It also reminds us that lifestyle measures-hydration, stress reduction, caffeine moderation-can sometimes tip the scales back toward rhythm stability.
Yet, for those with frequent or symptomatic episodes, the next step often involves pharmacologic therapy or catheter ablation, tools that have dramatically improved outcomes over the past decades.
In summary, this interactive guide is a beacon for both patients and clinicians, illuminating the path through the maze of supraventricular tachycardia with clarity, compassion, and scientific rigor.
ADam Hargrave
October 31, 2025 AT 08:18Oh great, another “DIY diagnosis”-because who needs doctors when you have a JavaScript wizard? 😏
Rohit Poroli
November 4, 2025 AT 12:18The algorithmic stratification here leverages hemodynamic thresholds and electrophysiological markers to delineate AVNRT from orthodromic AVRT, which is particularly salient when considering substrate modification strategies.
Incorporating delta wave detection aligns with the classic accessory pathway paradigm, facilitating risk stratification for sudden cardiac death.
Overall, the interface provides a pragmatic decision‑support matrix, albeit with the caveat that invasive EP study remains the gold standard.
William Goodwin
November 8, 2025 AT 16:18Behold, dear readers, a digital oracle that translates the cryptic dance of atrial impulses into something we mere mortals can grasp! 🌟
From the flutter of a rapid heartbeat to the subtle whisper of a delta wave, this tool paints a vivid tableau of arrhythmic intrigue.
It reminds us that medicine is both art and science, and that even the most bewildering ECG can be tamed with a few clicks.
Use it, share it, and may your rhythms stay steady. 🙏
Claus Rossler
November 12, 2025 AT 20:18While the theatrical flair is appreciated, one must caution against reducing complex electrophysiology to a “digital oracle.”
The nuances of concealed pathways and autonomic modulation cannot be fully captured by checkbox logic.
Thus, the tool serves as a superficial primer at best, not a substitute for rigorous electrophysiological mapping.
chris mattox
November 17, 2025 AT 00:18Colors of language aside, this guide does a splendid job of weaving together symptomatology and ECG morphology into an accessible tapestry.
The phrasing feels fresh, like a palette of words that paints the picture of each SVT subtype vividly.
Keep the creative spirit alive-maybe add a visual of the accessory pathway for extra flair.
Jackson Whicker
November 21, 2025 AT 04:18Ah, the romance of “painting pictures” with cardiac rhythms-how delightfully poetic!
Yet, let us not forget that behind each metaphor lies a patient whose life may be imperiled by unchecked tachycardia.
Hence, while we applaud the aesthetic, we must also champion the urgency of timely intervention.
Audrin De Waal
November 25, 2025 AT 08:18Man, these SVT types sound like a secret code you need a decoder ring for.
If you’re not a med nerd, just trust the doc and don’t overthink it.
parag mandle
November 29, 2025 AT 12:18Delving into the electrophysiological underpinnings, one realizes that the accessory pathway in WPW essentially creates a shortcut-bypassing the AV node’s gatekeeping function.
This shortcut manifests as the characteristic delta wave, a hallmark that can be spotted even at rest.
Understanding this mechanism empowers clinicians to tailor ablation strategies with pinpoint precision.
Jessica Wheeler
December 3, 2025 AT 16:18The disclaimer is spot on, reminding users that self‑diagnosis can be a slippery slope-especially when typos creep in and muddle the medical terminology.
Still, the tool provides a valuable stepping stone toward informed discussions with healthcare providers.
Mikayla Blum
December 7, 2025 AT 20:18Exactly! Being precise with terms matters, but a little emoji can lighten the mood without sacrificing clarity 😊.
Great point about using this as a conversation starter with your doctor.
Jo D
December 12, 2025 AT 00:18Sure, let’s all trust a web form to triage our cardiac emergencies-because nothing says “clinical rigor” like clicking boxes while ignoring the chaotic reality of autonomic dysregulation.
Meanwhile, the jargon parade continues, leaving laypeople drowning in acronyms.
Sinead McArdle
December 16, 2025 AT 04:18I see your point, but the tool does offer a structured overview for patients seeking initial insight.
Katherine Krucker Merkle
December 20, 2025 AT 08:18Hey folks! I found the symptom checklist especially helpful-being able to tick off chest pain or light‑headedness made me feel more in control of what I’m experiencing.
Has anyone tried pairing this with a personal heart‑rate monitor? It could be a game‑changer for tracking episodes.
Mark Quintana
December 24, 2025 AT 12:18i think using a wearable is a great idea, but make sure the data syncs well with the app you use-otherwise you might get mismatched numbers and get confuseed.
Brandon Cassidy
December 28, 2025 AT 16:18In the grand tapestry of cardiac care, tools like this serve as threads that connect patient awareness to professional expertise.
When woven together with proper clinical guidance, they can enhance outcomes and foster collaborative decision‑making.