Antidepressant Symptom & Side Effect Tracker
Depression Symptoms Tracking (PHQ-9)
Rate how often you've been bothered by each problem in the last 2 weeks
PHQ-9 Score:
Antidepressant Side Effects Tracker (ASEC)
Rate the severity of each side effect (0 = none, 4 = severe)
ASEC Score:
Your Treatment Insight
What This Means
Enter your scores to see what they mean for your treatment.
Important: This tool is not a substitute for professional medical advice. Share your results with your healthcare provider for treatment decisions.
When you start an antidepressant, you’re not just hoping it works-you’re hoping it works without making you feel worse. But too often, patients are left guessing. Did the fog lift because the medicine helped, or because spring finally arrived? Is that dry mouth a side effect, or just stress? Without a clear way to measure progress, it’s easy to quit too soon-or stay stuck on a drug that’s doing more harm than good.
Why Tracking Matters More Than You Think
About 30-40% of people don’t get better on their first antidepressant. And 74% deal with at least one side effect. Yet, in many doctor’s offices, the check-in is still just: “How are you feeling?” That’s not enough. Research shows that using simple, structured tools to track symptoms and side effects can improve remission rates by 50-60%. This isn’t theory-it’s standard care in leading clinics, and it’s something you can use too.Two tools are used most often: the PHQ-9 and the Beck Depression Inventory (BDI). The PHQ-9 asks nine questions about sleep, energy, appetite, and mood, each scored from 0 to 3. A score of 15 or higher means moderate to severe depression. The BDI is longer-21 questions-but gives a more detailed picture. Both are free, quick to complete, and validated across thousands of patients. You don’t need a psychologist to use them. You just need consistency.
How to Track Your Symptoms Like a Pro
Start before you even take your first pill. Write down your baseline. What’s your lowest point? Can you get out of bed? Do you still enjoy coffee with a friend? Rate your mood on a scale of 1 to 10. Note any physical symptoms: dry mouth, nausea, dizziness, weight gain, sexual issues. Keep it simple. A notebook, a notes app, or a free tool like Moodfit or Sanvello works fine.Then, track every 2 to 4 weeks. Don’t wait until your next appointment. If you’re feeling worse after two weeks, that’s important. If your sleep improved but your anxiety spiked, that’s data. Write it down. By week 6, you should see at least a 50% drop in your PHQ-9 score if the medication is working. If not, your doctor needs to know-now, not in three months.
One patient, a teacher named Lisa, started sertraline and felt nothing but nausea and fatigue. She tracked her PHQ-9 weekly: 21 → 20 → 19 → 18. Her doctor assumed she wasn’t trying. But when she showed the numbers, they switched her to bupropion. Within three weeks, her score dropped to 9. She didn’t feel “cured,” but she could teach again. That’s what matters.
Side Effects Are Not Just ‘Normal’
Sexual dysfunction affects up to 61% of people on SSRIs. Weight gain? Common with mirtazapine and paroxetine. Insomnia? Escitalopram can cause it. But too many patients are told, “It’ll pass.” Sometimes it does. Sometimes it doesn’t. And if it doesn’t, you shouldn’t have to suffer silently.The Antidepressant Side-Effect Checklist (ASEC) lists 15 common side effects on a scale from 0 (none) to 4 (severe). Use it. Rate each one every two weeks. If your libido score stays at 4 for eight weeks, that’s not normal-it’s a signal. Bring this list to your appointment. Ask: “Is this fixable? Can we lower the dose? Switch meds?”
One man on fluoxetine reported losing interest in sex and gaining 15 pounds. His doctor said, “Lots of people deal with this.” He left. Six months later, he switched to vortioxetine after researching alternatives. His side effects vanished. His PHQ-9 dropped from 22 to 7. He didn’t give up-he just stopped accepting bad advice.
What Doctors Aren’t Telling You
Only 45% of U.S. psychiatrists use standardized scales regularly. In primary care, it’s worse-under 35%. Many doctors don’t have time. Others don’t know how. But you can fill the gap.Therapeutic Drug Monitoring (TDM) can measure exactly how much medication is in your blood. It’s not routine-but it should be if you’re not responding. Studies show 50-70% of people who don’t improve have drug levels too low-even if they’re taking their pills. TDM costs $50-$150 per test. It’s not covered by all insurance, but it’s worth asking for if you’ve tried two or more meds without success.
And don’t ignore the emotional side. Sometimes, people feel better functionally-getting out of bed, going to work-before their PHQ-9 score drops. That’s real progress. Don’t let a number tell you you’re failing if your life is improving. Ask your doctor: “Am I getting better in ways that matter?”
Your Toolkit: What Works
Here’s what you can do right now:- Download the PHQ-9 from the PHQ Screeners website and print it.
- Use a free app like Moodfit or Sanvello to log daily mood and side effects (even if just 5 minutes a week).
- Keep a simple journal: Date | Mood (1-10) | Side Effects | One thing I did today.
- At each appointment, hand your doctor your tracker. Say: “Here’s what’s changed.”
- If you’re not improving after 6 weeks, ask: “Should we check my blood level?” or “What’s the next option?”
One study found patients who tracked their symptoms weekly had 43% higher treatment satisfaction. Another showed those using apps had 32% better adherence. It’s not magic. It’s control.
When to Consider a Change
There’s no hard rule, but here are red flags:- Your PHQ-9 score hasn’t dropped by 50% after 6-8 weeks.
- Side effects are worse than your depression.
- You’ve tried two or more meds with no lasting benefit.
- You’ve stopped taking your pills because you couldn’t tolerate the side effects.
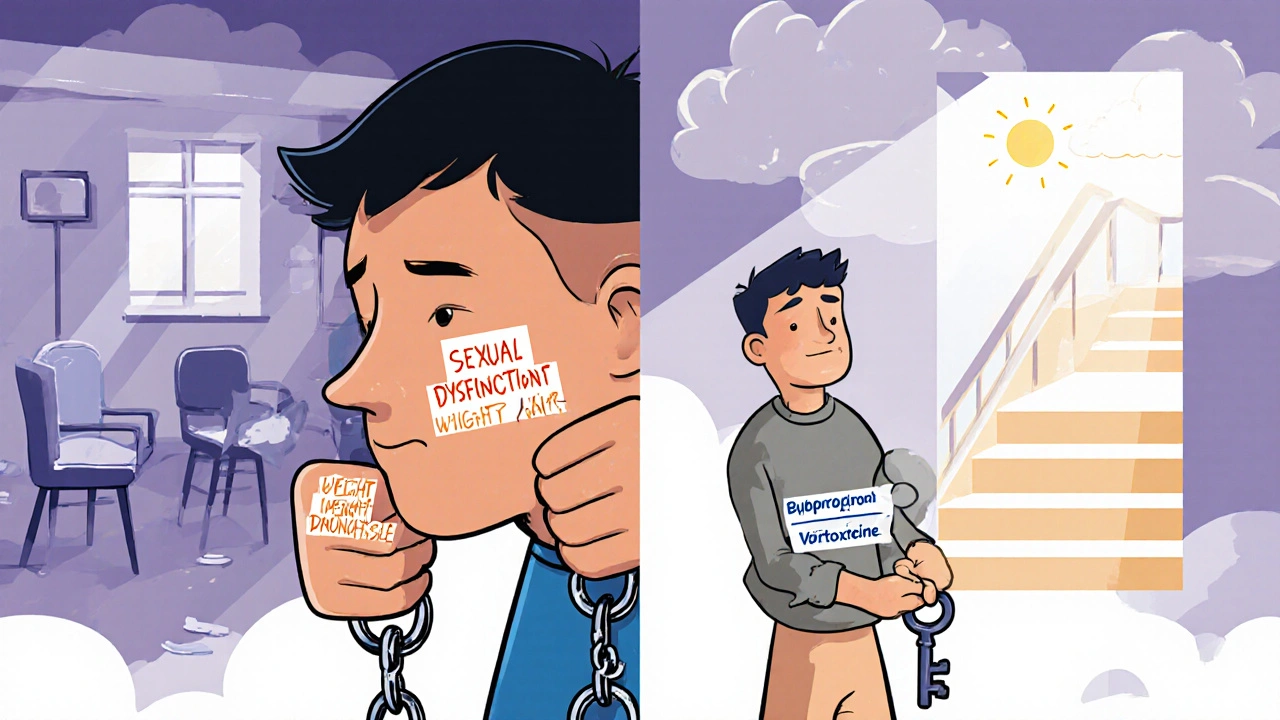
Don’t wait for your doctor to bring it up. If you’re stuck, ask about alternatives: switching to bupropion (less sexual side effects), adding cognitive behavioral therapy, or trying a newer option like vortioxetine or brexanolone. Pharmacogenetic testing (like GeneSight) can also help predict which drugs your body handles better-reducing side effects by 30% and boosting response by 20% in recent trials.
The Bigger Picture
The FDA cleared Rejoyn, the first digital therapeutic with built-in PHQ-9 tracking, in January 2024. That’s a sign: monitoring isn’t optional anymore. The American Psychiatric Association now requires it in all treatment plans. The question isn’t whether you should track-it’s whether you’re doing it right.Antidepressants aren’t quick fixes. They’re tools. And like any tool, they work best when you know how to use them. You’re not just taking a pill-you’re managing a process. The more data you collect, the more power you have to ask the right questions, make informed choices, and finally find a treatment that fits your life-not the other way around.
How often should I track my mood and side effects on antidepressants?
Track your mood and side effects every 2 to 4 weeks during the first 8 to 12 weeks of treatment. This is when your doctor will decide whether the medication is working or needs adjustment. After that, monthly tracking is usually enough unless symptoms change. Daily logging in an app can help spot patterns, but formal scores like PHQ-9 should be done weekly or biweekly for accurate trends.
What if my doctor doesn’t use rating scales?
Bring your own tracking. Print out a PHQ-9 or BDI form and hand it to your doctor at each visit. Say: “I’ve been tracking my symptoms because I want to make sure we’re on the right path.” Most doctors will appreciate the initiative. If they resist, ask why. If they dismiss it, consider finding a provider who uses Measurement-Based Care-it’s becoming standard for a reason.
Can I stop my antidepressant if side effects are bad?
Never stop abruptly. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or brain zaps. Instead, track your side effects, then talk to your doctor about tapering slowly or switching to a different medication. Some side effects, like sexual dysfunction or weight gain, may improve with dose changes or a switch to bupropion or vortioxetine-both have lower rates of these issues.
Is therapeutic drug monitoring worth it?
If you’ve tried two or more antidepressants without improvement, yes. Studies show 50-70% of non-responders have drug levels below the therapeutic range-even when they take their pills correctly. TDM costs $50-$150 per test and isn’t always covered by insurance, but it can prevent months of trial and error. Ask your psychiatrist or a psychiatric pharmacist if it’s right for you.
Do apps like Moodfit really help?
Yes. A 2023 study found users of Moodfit had 32% better medication adherence over six months. Apps help you notice patterns you’d miss-like mood drops after skipping sleep or increased anxiety after caffeine. They’re not perfect, but they’re better than nothing. Use them to gather data, not to diagnose yourself. Share the reports with your doctor.
What if I feel better but my PHQ-9 score hasn’t changed much?
That’s actually common. Some people improve functionally-going to work, socializing, sleeping better-before their symptom scores drop. This is called functional recovery. It’s real progress. Tell your doctor: “I’m doing things I couldn’t before.” Don’t let a number dismiss your improvement. Sometimes, feeling “better” isn’t about scores-it’s about living again.
Are there antidepressants with fewer side effects?
Yes. Bupropion (Wellbutrin) has lower rates of sexual side effects and weight gain. Vortioxetine (Trintellix) is linked to less fatigue and better cognitive function. Mirtazapine can help with sleep but causes weight gain. SNRIs like venlafaxine may worsen blood pressure. There’s no universal “best,” but knowing your priorities-sleep? energy? sex life?-helps guide the choice. Talk to your doctor about matching the drug to your life, not just your diagnosis.


Monika Wasylewska
November 25, 2025 AT 13:48Just started tracking my mood with Moodfit after reading this. My PHQ-9 dropped from 18 to 12 in three weeks. I didn’t realize how much I’d normalized feeling numb. Thanks for the nudge to actually measure it.
It’s wild how much power comes from data. Not magic, just clarity.
Jackie Burton
November 25, 2025 AT 19:57Let’s be real-this is all corporate psych’s way of making you a data point. The FDA cleared Rejoyn? That’s not progress, that’s surveillance capitalism with a SSRIs sticker. They don’t care if you feel better-they care if you log it. Your PHQ-9 score is now a KPI for your soul.
And don’t get me started on GeneSight. It’s a $1200 placebo wrapped in genomics jargon. Big Pharma’s new opiate.
Philip Crider
November 26, 2025 AT 08:51Bro I tried tracking with Sanvello for 3 days and it made me feel worse 😅
Like, why am I rating my mood at 4am after a panic attack? Who designed this? It’s like a fitness tracker for your depression.
But then again-my doc actually looked at my sheet and switched me to bupropion. I haven’t cried in 2 weeks. So maybe the app’s trash but the system works? 🤷♂️
Also side note: I lost 10 lbs and got my sex drive back. Vortioxetine is the real MVP. 🙌
Diana Sabillon
November 27, 2025 AT 08:51I just wanted to say thank you for writing this. I’ve been on paroxetine for 11 months and felt so guilty for wanting to quit because I thought I was just being weak.
When I started using the ASEC checklist, I realized my libido score had been at 4 for 8 months. I showed it to my doctor and she didn’t blink. We switched me. It’s been 3 weeks-I’m not ‘fixed’ but I’m alive again.
You’re not alone. And your suffering isn’t normal. It’s data.
neville grimshaw
November 28, 2025 AT 07:42Oh wow. Another ‘track your feelings like a productivity guru’ manifesto. How very Silicon Valley.
I mean, sure, if you’re a data-driven robot who thinks depression is just a bug in your emotional OS, then yes-log every tear, every yawn, every moment you forgot your own name.
But what about the people who just need someone to sit with them in the dark? Not a spreadsheet. Not a chart. Just… presence?
Also, who the hell has time to fill out PHQ-9 every two weeks when you’re working two jobs and your kid has asthma? This isn’t self-help. It’s classist.
Carl Gallagher
November 29, 2025 AT 16:20I appreciate the intent here, really I do. But I think we need to be careful about how we frame this. Tracking is powerful, no doubt-but it’s not a substitute for systemic change. If your doctor doesn’t have 15 minutes to review your data, that’s a problem with the system, not you.
Also, not everyone has access to smartphones, stable internet, or the mental bandwidth to log their emotions. For some, just getting out of bed is the win.
And while I agree with the tools mentioned, I’d add one more: community. Talking to someone who’s been there-online forums, peer support groups-can be just as validating as a PHQ-9 score.
Don’t let data become another burden. Let it be a compass, not a cage.
bert wallace
December 1, 2025 AT 07:59My wife used to say I was ‘just lazy’ when I couldn’t get out of bed. Then I started tracking. Week 1: PHQ-9 24. Week 4: 19. Week 6: 11.
She didn’t believe me until I showed her the numbers. Now she helps me log it. We even made a little ritual-coffee, 5 minutes, scribble down how I feel.
It’s not about being perfect. It’s about not letting the fog convince you it’s permanent.
Also-yes, sexual side effects are real. And no, you shouldn’t have to suffer them in silence. I switched to bupropion. My libido came back. My marriage did too.
Neal Shaw
December 3, 2025 AT 01:36It’s worth noting that the 50-60% improvement in remission rates with structured tracking comes from RCTs conducted in academic medical centers with trained clinicians. In primary care, where most patients are treated, the effect size is significantly smaller-closer to 15-20%-due to inconsistent implementation.
Also, while PHQ-9 and BDI are validated, they’re not diagnostic. They’re screening tools. Misinterpretation is common. A score of 15 doesn’t equal ‘clinical depression’-it means ‘consider further evaluation.’
Therapeutic Drug Monitoring (TDM) is underutilized but not universally applicable. CYP2D6 polymorphisms affect metabolism, but not all drugs have clinically actionable thresholds. Bupropion, for example, lacks clear TDM guidelines.
Still, the core message stands: data informs decisions. Silence doesn’t.
Hamza Asghar
December 4, 2025 AT 23:27Oh wow. Another ‘just log your feelings and you’ll be fine’ fairy tale from someone who’s never had to live with this.
PHQ-9? BDI? You think your therapist cares about your 1-10 scale when they’re rushing between 8 patients an hour? Nah. They’re collecting checkboxes to justify insurance billing.
And GeneSight? That’s a scam. 30% reduction? In whose study? The one funded by the company selling the test?
Real talk: if you’re not improving, it’s not your fault. It’s your doctor’s failure. Stop blaming yourself. Stop logging. Stop being a lab rat.
Find a new doctor. Or don’t take the pill. Either way, don’t let this blog post make you feel guilty for being human.
Karla Luis
December 5, 2025 AT 11:41So I tracked for 6 weeks, switched meds, now I’m back to work and actually laughing again
and my doctor still said ‘good job’ like I just aced a pop quiz 😂