When your stomach is in knots, you’re rushing to the bathroom, or you’re constantly bloated, it’s easy to assume you have "bowel issues." But not all gut problems are the same. Two conditions-IBS and IBD-sound similar and share symptoms like diarrhea, cramps, and bloating. Yet they’re fundamentally different in cause, diagnosis, and long-term impact. Confusing them can lead to wrong treatments, unnecessary stress, or even dangerous delays in care.
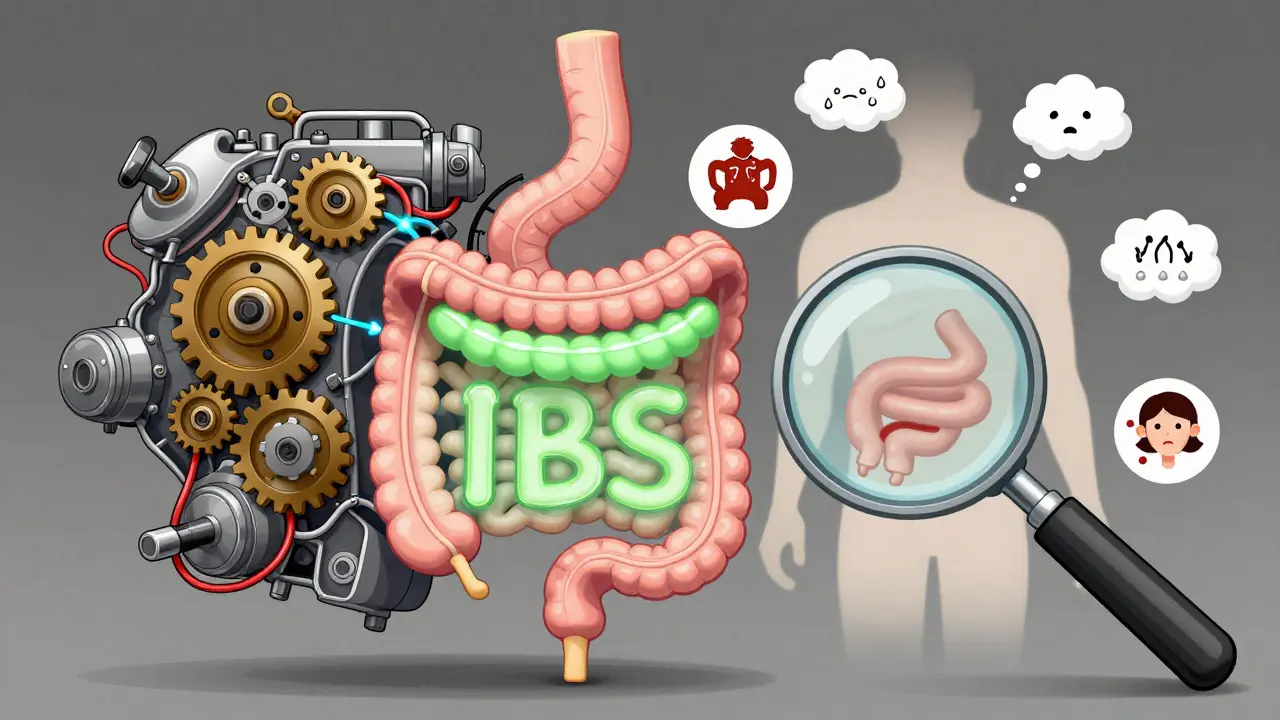
What Is IBS? A Functional Disorder Without Damage
Irritable Bowel Syndrome, or IBS, isn’t caused by inflammation, infection, or structural damage. It’s a functional disorder. That means your gut looks normal on scans and biopsies, but it doesn’t work right. Think of it like a misfiring engine: everything’s in place, but the signals are off. According to the Rome IV criteria (updated in 2016), IBS is diagnosed when you have abdominal pain at least one day a week for three months, along with changes in bowel habits. You might have diarrhea more often (IBS-D), constipation (IBS-C), or both (IBS-M). Around 76% of people with IBS report bloating. Nearly half notice mucus in their stool. Symptoms often flare after meals, during stress, or after certain foods. Crucially, IBS doesn’t cause bleeding, weight loss, or fever. If you’re losing weight without trying, or seeing blood in your stool, that’s not IBS. Those are red flags for something else. Doctors diagnose IBS by ruling out other conditions. There’s no single test. You’ll likely have blood work, stool tests, and maybe a colonoscopy-but all of them will come back normal. That’s not a failure of testing. It’s confirmation of IBS.What Is IBD? Inflammation That Damages Your Gut
Inflammatory Bowel Disease is not one condition. It’s two: Crohn’s disease and ulcerative colitis. Both involve chronic inflammation that physically damages the lining of your digestive tract. In Crohn’s disease, inflammation can hit anywhere from mouth to anus. It doesn’t just affect the surface-it digs deep into the gut wall. This can lead to ulcers, strictures (narrowing of the intestine), and fistulas (abnormal tunnels between organs). About 33% of people with Crohn’s develop strictures within 10 years. Around 17% get fistulas. Ulcerative colitis sticks to the colon and rectum. It causes continuous inflammation and ulcers on the innermost layer. Blood in the stool? That’s common-seen in 92% of ulcerative colitis patients at diagnosis. Black, tarry stools? That can mean bleeding higher up, seen in 15% of Crohn’s cases. IBD doesn’t just mess with your gut. It can trigger problems elsewhere: joint pain, eye inflammation (uveitis), skin rashes like erythema nodosum, and even liver issues. These are called extraintestinal manifestations. They’re rare in IBS.The Big Difference: Inflammation and Damage
This is where IBS and IBD split apart completely. IBS: No inflammation. No ulcers. No tissue damage. Your colon looks perfect under a scope. IBD: Inflammation is everywhere. Biopsies show immune cells attacking the gut lining. Blood tests show high C-reactive protein (CRP)-a marker of inflammation. Stool tests show elevated calprotectin, which signals active gut inflammation. A 2022 study in the American Journal of Gastroenterology found that 95% of IBD patients had fecal calprotectin levels above 250 µg/g. IBS patients? Their levels stayed below 50 µg/g-the same as healthy people. The CDC and Mayo Clinic both say it plainly: IBD causes structural damage. IBS does not. That’s why IBD can lead to cancer risk. After 10 years of pancolitis (ulcerative colitis affecting the whole colon), the risk of colorectal cancer jumps by 2% per year. IBS carries zero cancer risk.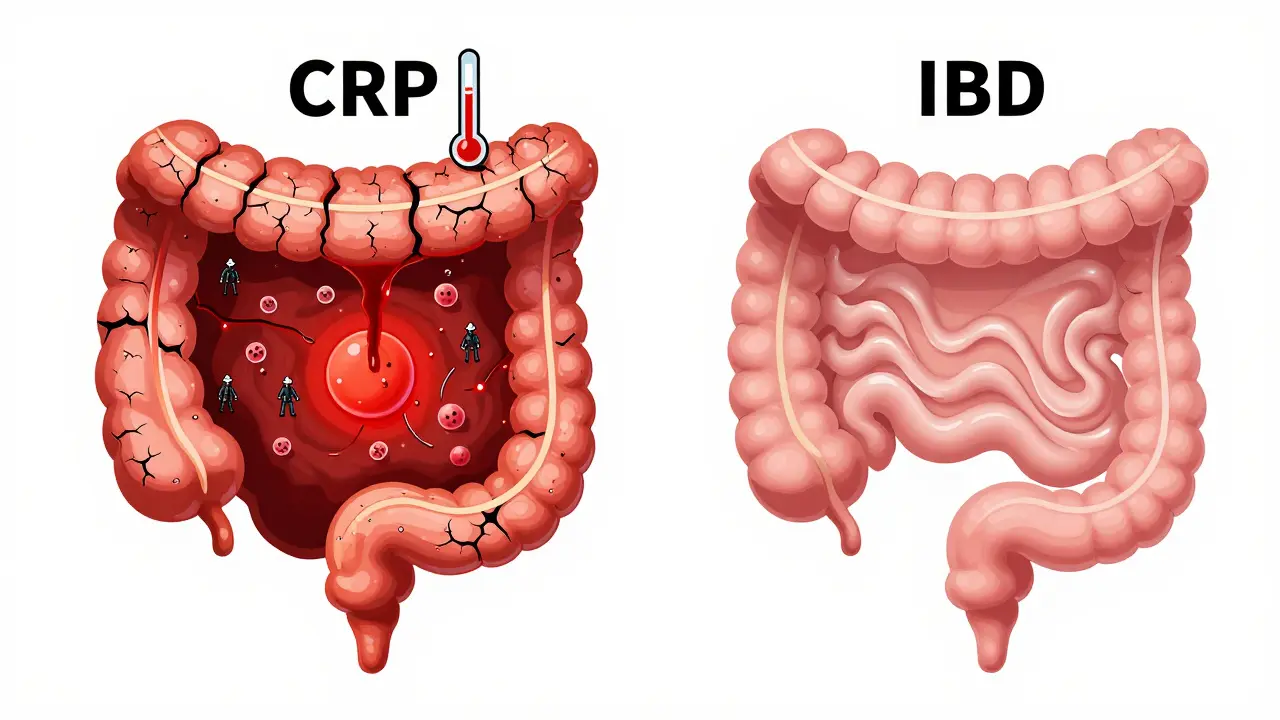
How Are They Diagnosed?
IBS diagnosis is like a detective game. You eliminate everything else. If you’re under 50, have no family history of colon cancer, no weight loss, no bleeding, and no fever-your symptoms fit IBS if they match the Rome IV criteria. IBD diagnosis is more aggressive. Doctors don’t wait to rule things out. They look for proof of damage. That means:- Colonoscopy with biopsies-showing inflamed, ulcerated tissue
- MRI enterography-detecting thickened bowel walls or fistulas in Crohn’s
- Blood tests-high CRP, low hemoglobin (anemia), elevated white blood cells
- Fecal calprotectin-over 250 µg/g confirms active inflammation
Treatment: Different Goals, Different Tools
IBS treatment is about managing symptoms, not curing disease. You can’t fix what isn’t broken. So doctors focus on what triggers your gut:- Low-FODMAP diet: Studies show it reduces symptoms in 76% of IBS patients. It cuts out fermentable carbs found in onions, garlic, dairy, and certain fruits.
- Low-dose antidepressants: Not because you’re depressed. These drugs (like amitriptyline) calm overactive nerves in the gut. They cut pain by 50% in 60% of users.
- Gut-targeted meds: Drugs like eluxadoline help with IBS-D. Linaclotide helps IBS-C.
- Anti-TNF drugs: Infliximab puts 50-60% of Crohn’s patients into remission within 14 weeks.
- Biologics: Vedolizumab targets gut-specific immune cells. It induces remission in nearly half of ulcerative colitis patients after a year.
- Corticosteroids: Effective for flares, but not for long-term use. Side effects include bone loss, diabetes, and mood swings.