Arthritis Massage Effectiveness Calculator
Imagine easing the constant ache in your hands or knees without popping a pill. Recent surveys show that over 25% of arthritis patients turn to massage therapy for the very reason - they want a gentler way to feel better.
Quick Takeaways
- Massage improves blood flow, which can lower joint inflammation.
- It triggers endorphin release, naturally dulling pain.
- Regular sessions boost range of motion and reduce muscle tension around affected joints.
- Most styles are safe for both osteoarthritis and rheumatoid arthritis when proper precautions are followed.
- Combine massage with medication and exercise for the strongest, long‑lasting relief.
What is Massage Therapy?
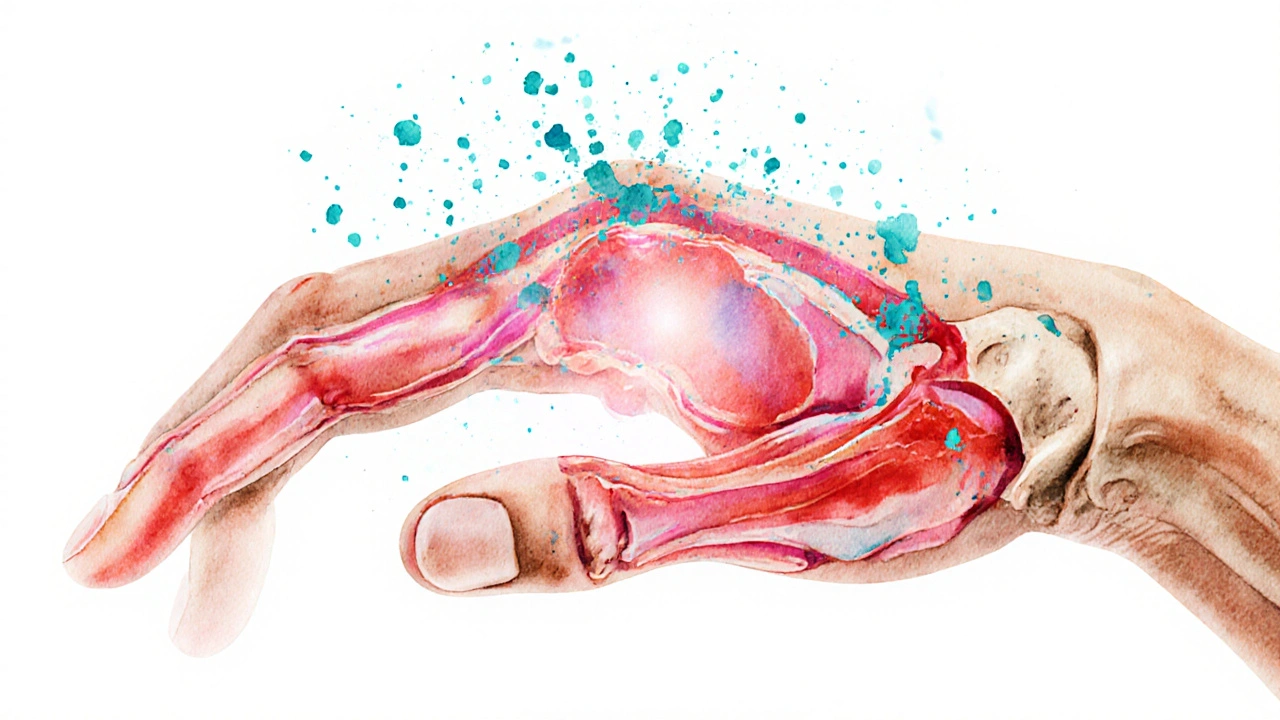
Massage therapy is a hands‑on treatment that manipulates muscles, tendons, and fascia to promote health and relieve discomfort. Therapists use pressure, rhythm, and movement to affect the body’s soft tissues.
Understanding Arthritis
Arthritis refers to inflammation of one or more joints, causing pain, stiffness, and reduced mobility. The two most common forms are osteoarthritis, which results from wear‑and‑tear, and rheumatoid arthritis, an autoimmune condition that attacks joint linings.
How Massage Helps Arthritis Sufferers
Massage tackles arthritis from several angles:
- Boosting circulation: By increasing blood flow, massage delivers oxygen and nutrients to cartilage while flushing out waste products that fuel inflammation.
- Reducing inflammatory markers: Studies have shown lowered levels of C‑reactive protein (CRP) after a series of weekly sessions.
- Releasing endorphins: Endorphins are natural pain‑killing chemicals produced by the brain surge during gentle pressure, creating a soothing sensation.
- Relaxing surrounding muscles: Tight muscles pull on joints, increasing stress. Massage loosens these muscles, allowing joints to move more freely.
- Lowering stress hormones: Cortisol drops after a session, which can indirectly lessen joint swelling.
Massage Techniques Most Effective for Arthritis
Not every massage style suits every arthritic joint. Here’s a quick guide:
- Swedish massage: Light to moderate strokes; ideal for beginners and people with mild joint pain.
- Deep‑tissue massage: Targets deeper muscle layers; best for chronic stiffness but should be moderated to avoid aggravating inflamed tissue.
- Myofascial release: Focuses on connective tissue; helps improve joint range of motion especially in the hands and feet.
- Trigger‑point therapy: Releases tight spots that refer pain to surrounding areas, useful for knee and shoulder arthritis.
Therapists often combine these methods, tailoring pressure based on the client’s pain threshold and joint condition.
Evidence from Clinical Research
Real‑world data backs up the anecdotal success stories:
- A 2023 randomized controlled trial involving 120 osteoarthritis patients found that 8 weeks of twice‑weekly Swedish massage reduced pain scores by an average of 30% compared to a control group.
- Research published in the Journal of Rheumatology (2022) reported a 15% drop in CRP levels among rheumatoid arthritis participants after a six‑session myofascial program.
- Longitudinal surveys from the American College of Rheumatology indicate that patients who supplement medication with regular massage experience a 20% slower progression of joint stiffness over two years.
Safety Guidelines and Contra‑indications
Massage is generally safe, but certain conditions need special attention:
- Blood‑thinning medication: Use gentle strokes and avoid deep pressure over large blood vessels.
- Severe flare‑ups of rheumatoid arthritis: Wait until inflammation subsides before scheduling a session.
- Skin infections or open wounds: These areas should be avoided to prevent spreading bacteria.
- Recent joint surgery: Follow your surgeon’s timeline; most advise waiting 6‑8 weeks.
Always share your medical history with the therapist and ask for modifications if anything feels uncomfortable.
Integrating Massage into a Comprehensive Arthritis Plan
Think of massage as a piece of a larger puzzle that includes medication, exercise, and diet. Here’s how to make it work:
- Schedule massage sessions on days when you have lighter medication doses to gauge combined effects.
- Combine with low‑impact activities like swimming or tai chi; the increased flexibility from massage makes these exercises easier.
- Track pain levels before and after each session in a simple journal; over time you’ll see patterns that guide frequency.
- Discuss findings with your rheumatologist - many doctors welcome complementary therapies when they’re documented.
Choosing the Right Therapist
Credentials matter, especially for chronic conditions:
- Look for a Licensed Massage Therapist (LMT) who has completed at least 500 hours of training.
- Therapists with additional certification in Medical Massage or experience treating arthritis patients are ideal.
- Ask about their familiarity with specific techniques like myofascial release or trigger‑point therapy.
- Read reviews focusing on timeliness, communication, and how well they adapt pressure levels.
Massage Therapy vs. Common Arthritis Treatments
| Aspect | Massage Therapy | NSAIDs (e.g., ibuprofen) | Physical Therapy |
|---|---|---|---|
| Onset of relief | 15‑30minutes after session | 30‑60minutes after dose | Weeks of consistent treatment |
| Typical duration of effect | Several days to a week | 4‑6hours | Long‑term improvement with regular visits |
| Side‑effect profile | Rare; occasional soreness | Stomach irritation, cardiovascular risk | Low; possible muscle soreness |
| Cost per session (US$) | 70‑120 | 0‑20 (over‑the‑counter) | 80‑150 |
| Best for | Immediate comfort, stress reduction, joint mobility | Acute inflammation, rapid pain spikes | Strength building, gait correction, long‑term function |
Key Takeaways for Everyday Use
- Start with short, 30‑minute Swedish sessions and gauge how your joints respond.
- Progress to deeper techniques only after inflammation is under control.
- Keep a simple log: date, technique, pressure level, pain score (0‑10), and any side effects.
- Share the log with your healthcare team to fine‑tune medication dosages.
- Remember that consistency beats intensity - regular weekly massages yield the best results.

Frequently Asked Questions
Can massage replace my arthritis medication?
Massage is a complementary tool, not a substitute. It can reduce pain and improve function, but most patients still need prescribed meds to control inflammation.
How often should I get a massage?
For moderate arthritis, one to two 45‑minute sessions per week work well. Adjust frequency based on pain levels and therapist advice.
Is deep‑tissue massage safe for swollen joints?
During acute swelling, stick to gentle methods like Swedish or light myofascial work. Deep pressure can aggravate inflamed tissue.
Do I need a special licensure to treat arthritis patients?
Therapists should hold an LMT license, and many rheumatology clinics prefer those with additional training in medical or orthopedic massage.
What should I do if I feel pain during a session?
Speak up immediately. A good therapist will adjust pressure or technique. Persistent sharp pain may signal an underlying issue that needs medical review.


Kevin Cahuana
October 2, 2025 AT 22:47I've found that a gentle Swedish massage can really loosen up stiff joints, especially around the knees and hips. The rhythmic strokes help increase circulation, which in turn reduces swelling and pain. If you keep a regular schedule-like once a week-you'll notice a steadier improvement over a few months. Just make sure you tell the therapist about any specific flare‑ups so they can adjust the pressure.
Danielle Ryan
October 7, 2025 AT 00:00Oh my gosh!!! This article totally blew my mind!!! Who knew that rubbing muscles could actually calm arthritis pain!!! It’s like magic ✨✨✨-you just have to pick the right style and keep at it!!!
Robyn Chowdhury
October 11, 2025 AT 01:14While the evidence for massage as a sole treatment remains modest, adjunctive therapy can complement pharmacological regimens. Patients should consult physicians before initiating any new modality. 🤔
Deb Kovach
October 15, 2025 AT 02:27There are several massage techniques that target arthritis symptoms differently. Swedish massage uses long, gliding strokes that improve overall blood flow, which can lessen joint stiffness. Deep‑tissue focuses on deeper muscle layers, often relieving chronic tension that aggravates pain. Myofascial release works on the connective tissue, helping to restore range of motion around the joint. Trigger point therapy isolates specific knots that may refer pain to the arthritic area. Combining these approaches with a consistent frequency-ideally weekly-has shown the best outcomes in clinical observations.
Sarah Pearce
October 19, 2025 AT 03:40i think massage r good for arthritis!!!
Ajay Kumar
October 23, 2025 AT 04:54Exactly, Kevin! Staying consistent is key, and communicating your pain levels helps the therapist fine‑tune each session. I’ve seen friends who started with monthly visits and gradually moved to weekly once they felt the relief kicking in.
Richa Ajrekar
October 27, 2025 AT 05:07While the article mentions “potential benefits,” it fails to cite any peer‑reviewed studies. Moreover, the phrasing “massage can help arthritis relief” is misleading without specifying the degree of relief.
Pramod Hingmang
October 31, 2025 AT 06:20Great breakdown, Deb. Each technique indeed has its niche, and mixing them can address both surface and deep‑seated tension.
Benjamin Hamel
November 4, 2025 AT 07:34Honestly, I’m skeptical about the hype surrounding massage for arthritis. Most of the relief people report can be chalked up to the placebo effect or temporary increased blood flow, which doesn’t address the underlying inflammation. You could argue that taking a short walk or doing low‑impact exercises yields comparable benefits without the cost. Plus, if you’re not careful, aggressive manipulation might aggravate the joint rather than soothe it. So while a gentle session may feel nice, I’d caution anyone from relying on it as a primary treatment.
Christian James Wood
November 8, 2025 AT 08:47Let’s get something straight: the notion that massage is a miracle cure for arthritis is pure marketing fluff. First, the inflammatory process in arthritic joints is driven by biochemical pathways that a therapist’s hands simply cannot alter. Second, studies that claim “significant pain reduction” often suffer from tiny sample sizes and lack proper control groups. Third, any transient relief you feel is usually due to increased endorphin release, which fades within hours. Fourth, the financial burden of weekly professional massages can quickly outpace the modest gains reported. Fifth, many patients misinterpret short‑term flexibility improvements as long‑term disease modification, which is a dangerous misconception. Sixth, there’s a real risk of over‑pressurizing fragile joints, leading to micro‑injuries that exacerbate swelling. Seventh, insurance companies rarely cover these sessions, leaving patients to pay out‑of‑pocket for a service that lacks robust evidence. Eighth, the time commitment required for consistent therapy often distracts from proven interventions like physical therapy and strength training. Ninth, relying on massage may cause some individuals to neglect essential lifestyle changes such as diet and weight management. Tenth, the placebo effect, while powerful, should not be glorified as a cure. Eleventh, the industry often uses anecdotal testimonials in place of rigorous data, which is scientifically irresponsible. Twelfth, if you truly want to mitigate arthritis progression, focus on anti‑inflammatory medications prescribed by a rheumatologist. Thirteenth, incorporate low‑impact aerobic activities that have been shown to improve joint health. Fourteenth, consult a qualified health professional before adding any new modality. Fifteenth, understand that massage can be a complementary comfort, but not a standalone solution. Sixteenth, in the end, a balanced approach that combines evidence‑based treatments with occasional soothing sessions is the only rational path forward.
Rebecca Ebstein
November 12, 2025 AT 10:00Love the thoroughness, Christian! 🎉 Even if it’s not a cure‑all, a soothing massage can still lift spirits and make daily movement easier. 😊
Sandy Gold
November 16, 2025 AT 11:14From an academic standpoint, the discourse around massage therapy often neglects the nuanced interplay between mechanotransduction and synovial fluid dynamics. A rigorous meta‑analysis would likely reveal a modest effect size at best, necessitating cautious interpretation of anecdotal reports.