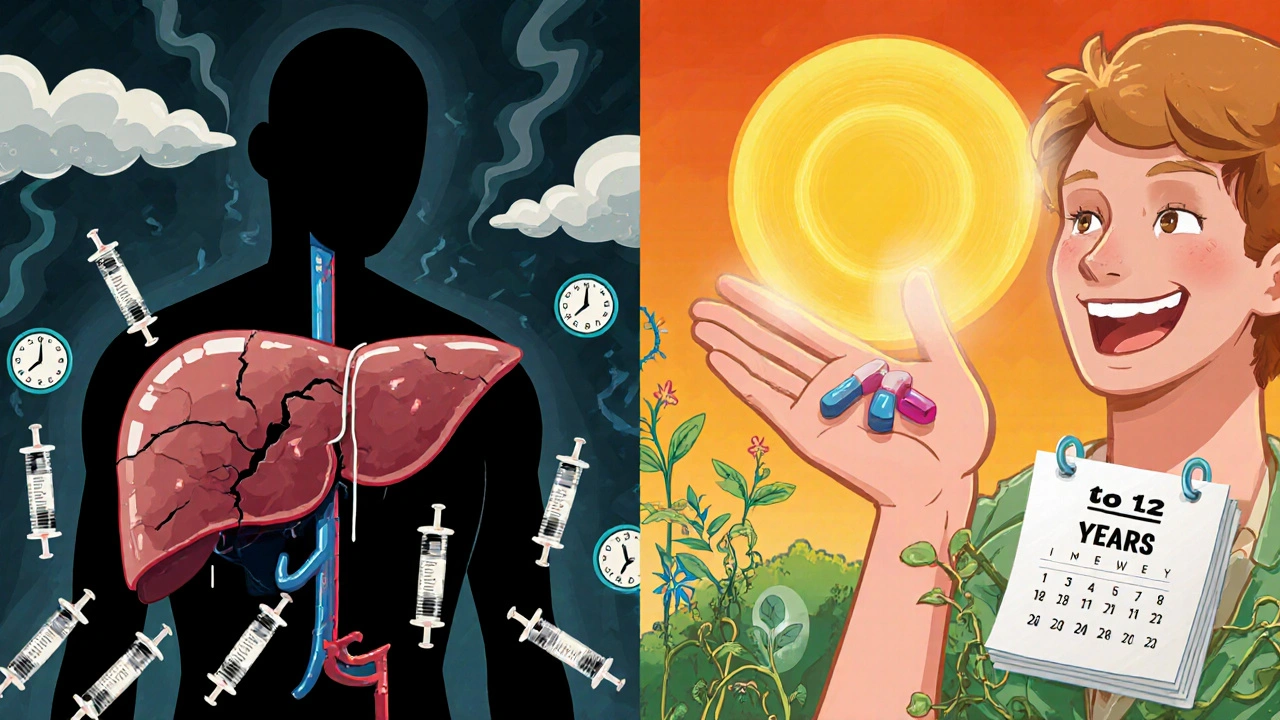
Before direct-acting antivirals (DAAs), hepatitis C was a slow, silent killer. People waited years for a liver transplant. Others lived with constant fatigue, brain fog, and the fear that their liver would fail. The old treatment? Weekly injections, months of flu-like symptoms, depression, and a 50% chance of cure at best. Today, that’s all changed. If you’re diagnosed with hepatitis C, you now have a better than 95% chance of being cured-with just 8 to 12 weeks of pills. No shots. No hospital visits. No unbearable side effects.
How DAAs Actually Work
Direct-acting antivirals don’t boost your immune system like old treatments did. Instead, they attack the hepatitis C virus directly. They block three key proteins the virus needs to copy itself: NS3/4A protease, NS5A, and NS5B polymerase. Each drug targets one of these, and when combined, they shut down the virus completely.
Before DAAs, doctors used interferon and ribavirin. Those drugs tried to force your body to fight the virus, but they often made you sicker than the disease. DAAs are different. They’re targeted, precise, and gentle. A person with hepatitis C today takes one or two pills a day, usually for just three months. That’s it.
Cure Rates: More Than 95%
Multiple studies across the U.S. and globally confirm the same thing: DAAs cure over 95% of people. One study of more than 6,600 insured patients in the U.S. found that 97.3% achieved sustained virologic response (SVR)-the medical term for being cured. That means the virus disappeared from their blood 12 weeks after finishing treatment and stayed gone.
This high success rate holds true even in tough cases. People with cirrhosis, HIV co-infection, or kidney disease all respond just as well. A 2023 study of 238 patients showed 92.8% achieved SVR. Another looked at people with HIV and hepatitis C together and found cure rates matched those of people without HIV. That’s huge. It means no one is too sick or too complex to be treated.
Real-World Results vs. Clinical Trials
Some people worry that clinical trial numbers are too good to be true. But real-world data backs it up. In clinics, community health centers, and even prisons, DAAs work just as well. The difference? In trials, patients are closely monitored. In the real world, they might miss a dose or forget to refill. Even then, cure rates stay above 90%.
One big reason? Modern regimens are pangenotypic. That means they work against all major strains of hepatitis C (genotypes 1 through 6). You don’t need a complicated blood test to figure out your genotype before starting treatment. Just one pill combo works for almost everyone.
Key DAA Regimens in Use Today
There are three main DAA combinations used today, all approved by the FDA and recommended by the WHO:
- Sofosbuvir-velpatasvir (Epclusa): Works for all genotypes. Often used for 12 weeks.
- Glecaprevir-pibrentasvir (Mavyret): Also pangenotypic. Can be taken for just 8 weeks in people without cirrhosis.
- Sofosbuvir-velpatasvir-voxilaprevir (Vosevi): Used when a prior DAA treatment failed.
These aren’t experimental. They’re the standard. In 2023, 91% of countries had registered at least one DAA. Over 68% of them offer insurance coverage or government reimbursement.
What Happens After You’re Cured?
Getting rid of the virus doesn’t just stop liver damage-it reverses it. Studies show that after SVR, liver inflammation drops. Scar tissue (fibrosis) improves. People who had cirrhosis before treatment see a 50% lower risk of liver cancer. Their risk of liver failure drops too.
But the benefits go beyond the liver. People who are cured have lower rates of kidney disease, diabetes, and even depression. One study found that the rate of chronic kidney disease dropped from 21 per 1,000 person-years in untreated people to just 14.7 per 1,000 in those who were cured.
And the long-term impact? Researchers estimate that if all eligible people in the U.S. were treated with DAAs, we could prevent over 450,000 hepatitis C-related deaths by 2050.
The Hidden Problem: Access and Equity
Here’s the hard truth: even with 97% cure rates, most people with hepatitis C still aren’t getting treated.
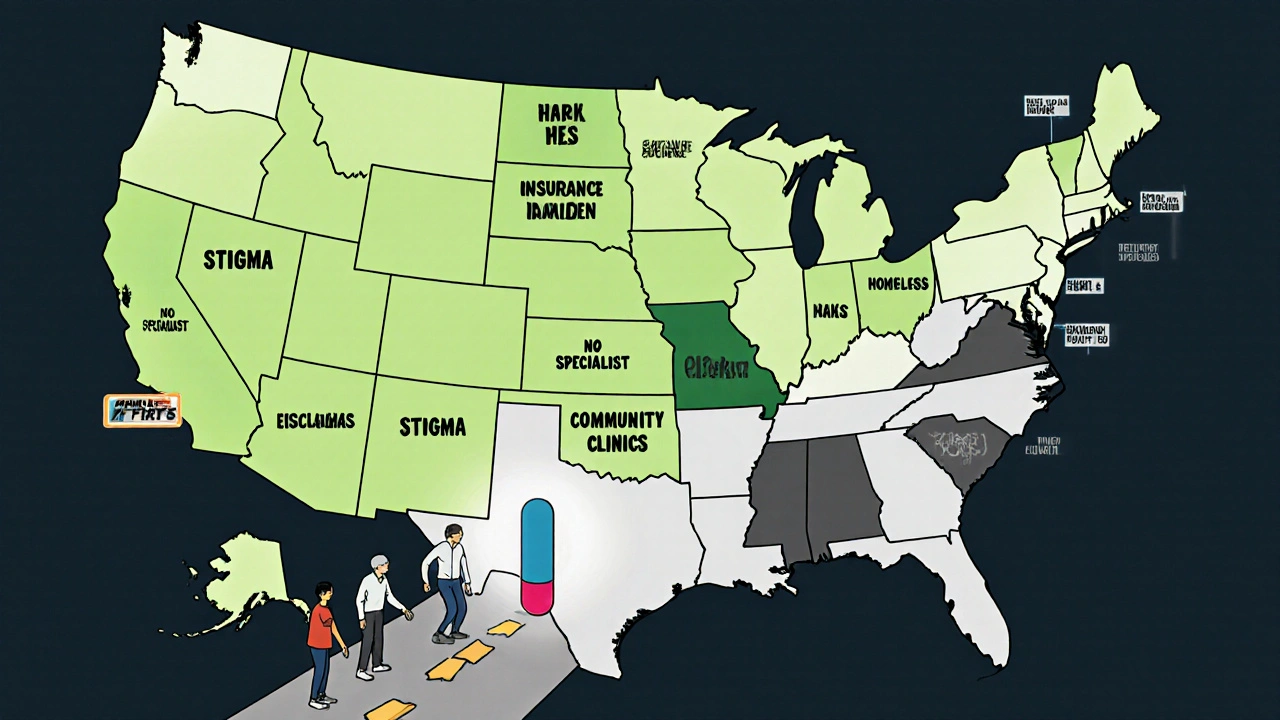
The CDC found that less than one in three insured Americans get DAA treatment within a year of diagnosis. Among Medicaid recipients, it’s worse-only 23% get treated. That’s not because the drugs don’t work. It’s because of bureaucracy, stigma, lack of awareness, and fragmented care.
Regional gaps are stark. People in the Northeast and Midwest are 20-30% more likely to get treated than those in the West-even after adjusting for income, race, and liver disease severity. Why? Some areas have better screening programs. Others have more providers trained to manage hepatitis C.
And then there’s the cost. When DAAs first came out in 2013, a 12-week course cost $84,000. Now, generic versions cost between $260 and $2,800 depending on where you live. But even at $2,800, many patients can’t afford it without insurance. In low- and middle-income countries, 61% of places that offer DAAs still require a specialist to prescribe them. That’s a huge barrier in places without enough liver doctors.
Who’s Still Being Left Behind?
Some of the people who need treatment the most are getting it the least.
Patients with decompensated cirrhosis (advanced liver failure) or hepatocellular carcinoma (liver cancer) are 30% less likely to get DAAs-even though studies show they benefit the most. Curing hepatitis C in these patients improves survival, reduces transplant needs, and lowers the chance of cancer spreading.
People who use drugs, are homeless, or are incarcerated also face major barriers. Stigma keeps them from seeking care. Clinics don’t always meet them where they are. But programs that bring treatment to needle exchanges, shelters, and jails are showing success. One study in a prison system cured 89% of participants within six months.
What Comes Next?
The WHO wants to eliminate hepatitis C as a public health threat by 2030. That means 90% fewer new infections and 65% fewer deaths. We have the tools. But we’re not using them fast enough.
The future lies in simplifying care. More countries are letting nurses, pharmacists, and primary care doctors prescribe DAAs. No more waiting months to see a liver specialist. Some places are even offering at-home testing and telehealth follow-ups.
Research continues. Scientists are testing even shorter treatments-some as short as four weeks. Others are looking at combination therapies that could work for people who’ve failed multiple rounds of DAAs.
But the biggest step forward won’t come from a new drug. It’ll come from better screening. Right now, millions of people don’t know they have hepatitis C. They feel fine. Their liver looks normal on a basic ultrasound. But the virus is quietly damaging them.
One simple blood test can find it. And if you test positive? You can be cured in three months. No needles. No hospital stays. Just pills.
What Should You Do?
If you’ve ever had a blood transfusion before 1992, used injection drugs, gotten a tattoo in an unregulated setting, or were born between 1945 and 1965-you’re at risk. Get tested. It’s a one-time blood draw. No fasting. No pain.
If you’re diagnosed, don’t wait. Talk to your doctor about DAAs. Ask if your insurance covers them. If you’re on Medicaid, push for it. Many states have expanded access. If you’re uninsured, look for community health centers or nonprofit programs that offer free or low-cost treatment.
Hepatitis C is no longer a death sentence. It’s a curable infection. But only if you know your status-and act on it.
Can hepatitis C come back after being cured with DAAs?
Once you achieve sustained virologic response (SVR)-meaning the virus is undetectable in your blood 12 weeks after finishing treatment-it’s considered cured. The chance of the virus returning is less than 1%. But you can get reinfected if you’re exposed again, such as through sharing needles or unprotected sex with someone who has hepatitis C. That’s why prevention after cure still matters.
Do DAAs work for everyone, including older adults or people with other health conditions?
Yes. DAAs are safe and effective for people over 65, those with kidney disease, HIV co-infection, obesity, and even those who’ve had liver transplants. Drug interactions are rare, and side effects are mild-usually just fatigue or headache. Doctors check for interactions with other medications (like statins or blood thinners), but most people can take DAAs without issue.
How long does it take to feel better after starting DAAs?
Many people notice improvements within weeks. Fatigue, brain fog, and joint pain often start to lift after the first month. But the real healing happens over months and years as the liver repairs itself. Even if you feel fine, the virus is still damaging your liver. That’s why completing the full course is critical-even if you feel great.
Are there any side effects from DAAs?
Side effects are rare and mild. The most common are headache, tiredness, and nausea-usually gone by week two. Unlike interferon, DAAs don’t cause depression, severe anemia, or thyroid problems. In clinical trials, fewer than 3% of people stopped treatment because of side effects.
Can I drink alcohol after being cured of hepatitis C?
You can, but it’s not recommended. Even after cure, your liver may still have some scarring. Alcohol can worsen that damage over time and increase your risk of liver cancer. If you had cirrhosis before treatment, doctors strongly advise avoiding alcohol completely. For others, moderation is key-no more than one drink a day.
Do I need to get tested again after being cured?
Yes. You’ll get a follow-up test 12 weeks after finishing treatment to confirm SVR. After that, you don’t need routine HCV testing unless you’re re-exposed. But if you had cirrhosis before cure, you’ll still need regular liver cancer screening (ultrasound every 6 months) because your risk doesn’t drop to zero.

Evan Brady
November 18, 2025 AT 07:31DAAs are a miracle, no doubt. I was diagnosed in 2018, took Epclusa for 12 weeks, and now I feel like I’ve been rebooted. No more brain fog, no more waking up exhausted. My liver enzymes are normal. It’s wild how something so simple-just pills-could erase years of silent damage. I wish I’d known sooner.
Ram tech
November 19, 2025 AT 01:0595% cure rate? lol. i think they just want us to take the pills so pharma can keep sellin’ em. my cousin took it and still got liver probs. maybe it dont work for everyone. also, why do they never talk about the side effects? i heard people get real depressed. they just hide it.
Jenny Lee
November 21, 2025 AT 00:14Just got cured last month. Best decision I ever made. Seriously. Go get tested.
Erica Lundy
November 21, 2025 AT 03:46The triumph of DAAs is not merely pharmacological-it is epistemological. We have shifted the paradigm of viral disease from one of chronic management to one of definitive eradication. Yet, this very success exposes the fragility of our social infrastructure: the disjunction between medical capability and distributive justice. Why, in a world where cure is nearly guaranteed, do we allow stigma, bureaucracy, and geographic arbitrariness to determine who lives and who languishes? The virus is not the enemy anymore. The system is.
Kevin Jones
November 21, 2025 AT 22:56Let’s be real: DAAs are a pangenotypic game-changer. NS5A inhibitors? Check. NS3/4A protease blockade? Check. SVR rates above 97% in real-world cohorts? That’s not a trial-it’s a revolution. But the real bottleneck isn’t the drug. It’s the provider gap. Primary care needs to own this. No more gatekeeping by hepatologists. We’re talking about a condition that affects 2.4M Americans. You can’t treat it one specialist at a time.
Premanka Goswami
November 22, 2025 AT 20:34They’re telling you it’s cured… but what if the virus just goes dormant? What if it’s hiding in your DNA? They don’t want you to know the truth-Big Pharma and the CDC are working together to make you think you’re safe so they can keep pushing vaccines and surveillance. They don’t care about your liver. They care about control. And that ‘simple blood test’? It’s just the first step to tracking you. Don’t trust the system. Test yourself… with a home kit from a country that doesn’t report to the FDA.