Levothyroxine-PPI Absorption Impact Calculator
This tool estimates how taking proton pump inhibitors (PPIs) may affect your levothyroxine absorption and TSH levels. Based on clinical studies, PPIs can reduce levothyroxine absorption by up to 20-25%, potentially requiring dose adjustments.
If you’re taking levothyroxine for hypothyroidism and also use a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn, you might be unknowingly reducing the effectiveness of your thyroid medication. This isn’t a rare issue - nearly 2.7 million Americans on levothyroxine also take PPIs long-term. And for many, it’s causing their TSH levels to creep up without any obvious reason.
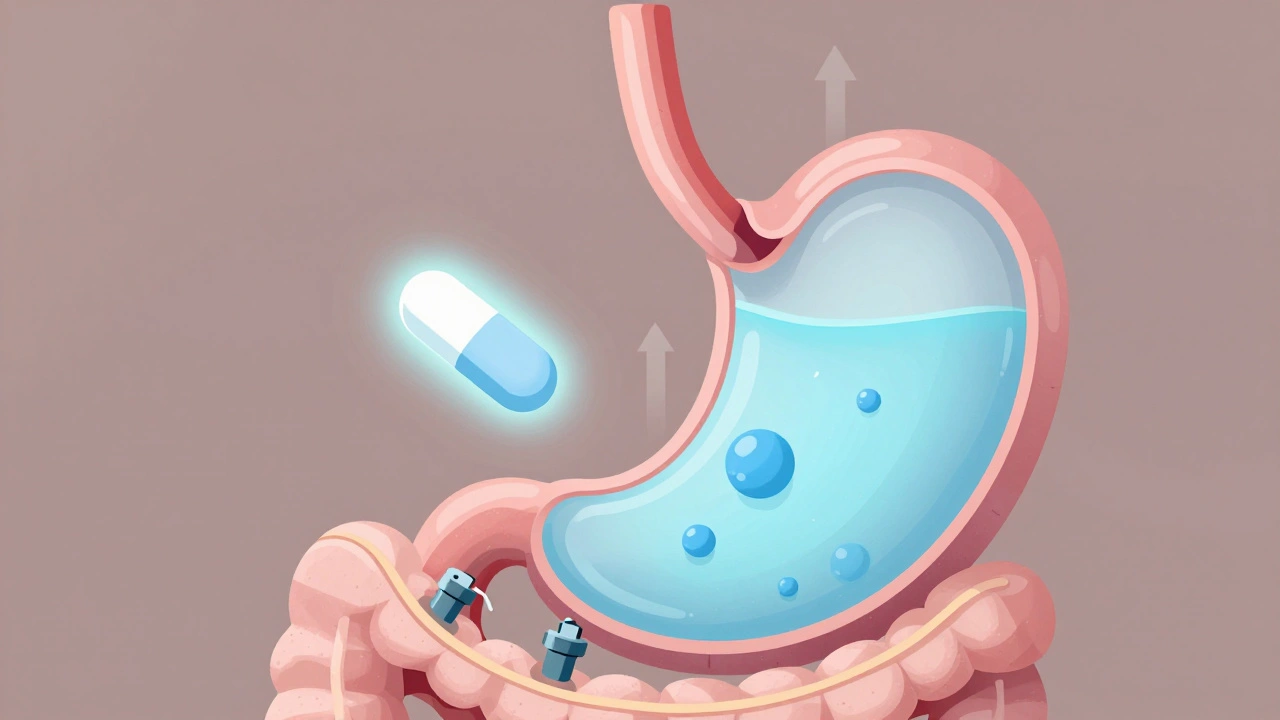
Why Levothyroxine Needs Stomach Acid
Levothyroxine isn’t like most pills. It doesn’t just dissolve and get absorbed anywhere in your gut. It needs an acidic environment - specifically, a stomach pH between 1 and 2 - to break down properly and enter your bloodstream. That’s why doctors tell you to take it on an empty stomach, first thing in the morning, with a full glass of water. No coffee, no food, no other meds for at least 30 to 60 minutes.
Proton pump inhibitors (PPIs) shut down your stomach’s acid production. They target the H+/K+ ATPase pumps in your stomach lining, the very same pumps that create the strong acid needed for digestion - and for levothyroxine to work. When you take a PPI, your stomach pH rises to 4 or higher. That’s not just less acidic; it’s practically neutral. And at that pH, levothyroxine doesn’t dissolve well. It passes through your gut mostly unchanged.
A 2021 systematic review in the Journal of General Internal Medicine looked at seven studies involving over 1,200 patients. Every single one found that people taking both levothyroxine and a PPI had higher TSH levels - meaning their thyroid hormone levels were dropping. Even patients who were stable on levothyroxine for years started showing signs of under-treatment after starting a PPI.
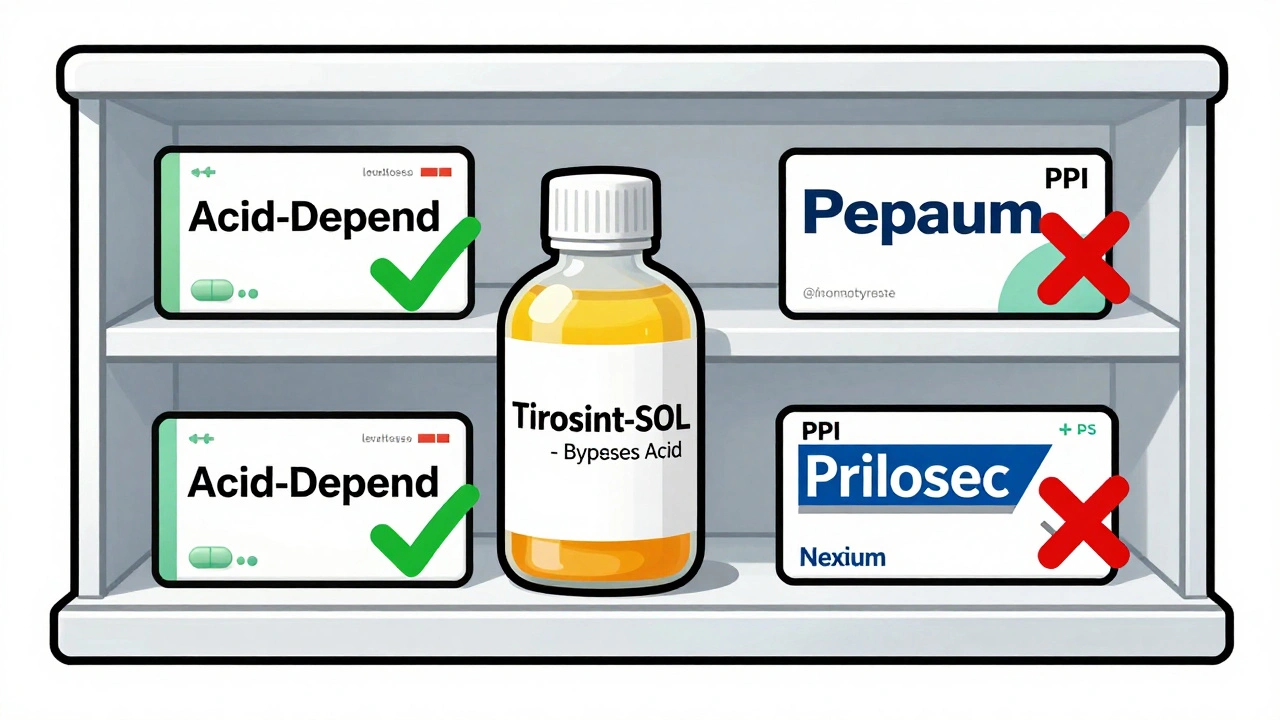
Which PPIs Cause the Most Problems?
All major PPIs interfere with levothyroxine absorption. That includes:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
- Pantoprazole (Protonix)
- Lansoprazole (Prevacid)
- Rabeprazole (Aciphex)
A 2023 study published in PubMed (PMID: 37259094) tested 40 mg of pantoprazole daily for six weeks in patients already on stable levothyroxine doses. TSH levels jumped significantly - even when the PPI was taken at night, 12 hours after levothyroxine. That’s important: timing doesn’t fix this. PPIs don’t just block acid for a few hours. They suppress it for up to 72 hours. So even if you take your thyroid pill in the morning and your PPI at night, your stomach is still too alkaline for levothyroxine to absorb.
What Happens When Levothyroxine Doesn’t Work
Low thyroid hormone levels don’t show up as sudden emergencies. They creep in slowly. Fatigue. Weight gain. Brain fog. Cold intolerance. Depression. These are the symptoms people often brush off as stress, aging, or lack of sleep. But for someone on levothyroxine, they could mean the drug isn’t being absorbed.
Reddit’s r/Hashimotos community analyzed 147 posts from users taking both medications. Of those, 68% reported needing higher levothyroxine doses after starting a PPI. Over 70% said they felt more tired. Nearly 60% gained weight despite no change in diet or exercise. These aren’t anecdotes - they’re real clinical signals.
And here’s the kicker: many doctors don’t test for this. If your TSH was normal last year and it’s slightly high now, they might just bump your dose by 12.5 mcg. But if you started a PPI six months ago, that’s likely the real cause - not your thyroid getting worse.

What Should You Do?
Don’t stop your PPI without talking to your doctor. But do take action.
- Get your TSH checked before starting a PPI, if possible. That gives you a baseline.
- Test again at 6 to 8 weeks after starting the PPI. If your TSH rose by more than 1.0 mIU/L, your levothyroxine dose probably needs adjusting.
- Don’t rely on timing. Taking levothyroxine four hours before or after a PPI won’t help. The acid suppression lasts too long.
- Ask about alternatives. H2 blockers like famotidine (Pepcid) don’t suppress acid as strongly or as long. A 2018 study showed no significant TSH changes when famotidine was used with levothyroxine.
Switching to Liquid Levothyroxine
There’s a solution that bypasses the stomach entirely: liquid levothyroxine. Tirosint-SOL is a brand-name liquid formulation made with glycerin instead of fillers that require acid to dissolve. It’s absorbed in the small intestine, not the stomach. That means PPIs don’t touch it.
A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed this. Patients switched from tablets to Tirosint-SOL while continuing PPIs - and their TSH levels returned to normal without any dose change.
The catch? Cost. Generic levothyroxine tablets cost $15 to $25 a month. Tirosint-SOL runs about $350. Insurance often covers it if you can prove the interaction - but many patients pay out of pocket. Some pharmacies offer savings cards. Others get it through patient assistance programs. It’s worth asking your endocrinologist or pharmacist about options.
What About Other Acid Reducers?
Antacids like Tums or Rolaids? They can interfere too - but only if taken at the same time. If you take them two hours after levothyroxine, the risk is low.
Calcium supplements? Big problem. They bind to levothyroxine and block absorption. Take them at least four hours apart.
Iron supplements? Same issue. Avoid taking them together.
But H2 blockers? They’re your friend. Famotidine reduces acid, but not as deeply or as long as PPIs. It’s a good middle ground if you need something for occasional heartburn and don’t want to mess with your thyroid levels.
When to Be Concerned
Short-term PPI use - say, two weeks for a bad bout of acid reflux - is unlikely to cause trouble. But if you’ve been on a PPI for more than three months, you’re in the danger zone. The American Thyroid Association and the American Association of Clinical Endocrinologists both recommend monitoring TSH every 6 to 8 weeks in patients on long-term PPIs.
And if your TSH keeps rising despite dose increases, it’s not you being non-compliant. It’s the drug interaction. Push for liquid levothyroxine or a switch to famotidine. Don’t settle for just increasing your dose over and over.
What’s Next?
The FDA is working on new labeling rules for thyroid medications that will require manufacturers to warn about PPI interactions. Phase 3 trials are testing enteric-coated levothyroxine tablets - designed to dissolve in the intestine, not the stomach. If they work, they could be a cheaper alternative to liquid formulations.
But here’s the reality: for now, if you’re on both drugs, you have to be proactive. Don’t wait for your doctor to catch it. Track your symptoms. Get your TSH tested. Ask about alternatives. Your thyroid doesn’t care how much you paid for your PPI - it only cares if it’s getting the hormone it needs.
Can I take levothyroxine and a PPI at the same time?
No, taking them together reduces levothyroxine absorption. Even separating them by hours doesn’t help because PPIs suppress stomach acid for up to 72 hours. The only reliable fix is switching to liquid levothyroxine or using an H2 blocker like famotidine instead.
Will my levothyroxine dose always need to be increased if I take a PPI?
Not always, but often. Studies show 15-20% of patients on long-term PPIs need a higher dose - typically 12.5 to 25 mcg more per day. Some patients stabilize with a single adjustment. Others need ongoing monitoring. The key is checking your TSH after starting the PPI, not assuming your current dose still works.
Is generic levothyroxine less affected by PPIs than brand names?
No. All tablet forms of levothyroxine - whether generic, Synthroid, or Levoxyl - rely on stomach acid for absorption. The issue isn’t the brand. It’s the tablet formulation. Only liquid formulations like Tirosint-SOL bypass this problem.
Can I switch from a PPI to an H2 blocker like Pepcid?
Yes, and many patients do. Famotidine (Pepcid) reduces acid less intensely and for a shorter time than PPIs. Studies show it doesn’t significantly affect levothyroxine absorption. It’s a good option for mild to moderate heartburn. But if you have severe GERD, you may still need a PPI - then liquid levothyroxine becomes the better choice.
How long does it take for TSH to return to normal after switching to liquid levothyroxine?
Most patients see their TSH levels drop back into target range within 4 to 6 weeks after switching from tablet to liquid levothyroxine. Some see changes in as little as two weeks. Your doctor will likely retest at 6 weeks to confirm stability. No dose change is usually needed - the liquid just works better.

Aileen Ferris
December 10, 2025 AT 01:21Ben Greening
December 11, 2025 AT 17:07Kaitlynn nail
December 12, 2025 AT 09:58Stephanie Maillet
December 12, 2025 AT 16:46David Palmer
December 12, 2025 AT 21:24Sarah Clifford
December 13, 2025 AT 12:36Regan Mears
December 13, 2025 AT 23:32Neelam Kumari
December 15, 2025 AT 14:29Doris Lee
December 17, 2025 AT 09:53Michaux Hyatt
December 18, 2025 AT 07:19Michelle Edwards
December 19, 2025 AT 19:26Frank Nouwens
December 20, 2025 AT 09:15Nikki Smellie
December 21, 2025 AT 02:47