PAD Treatment Decision Tool
Select Your Health Profile
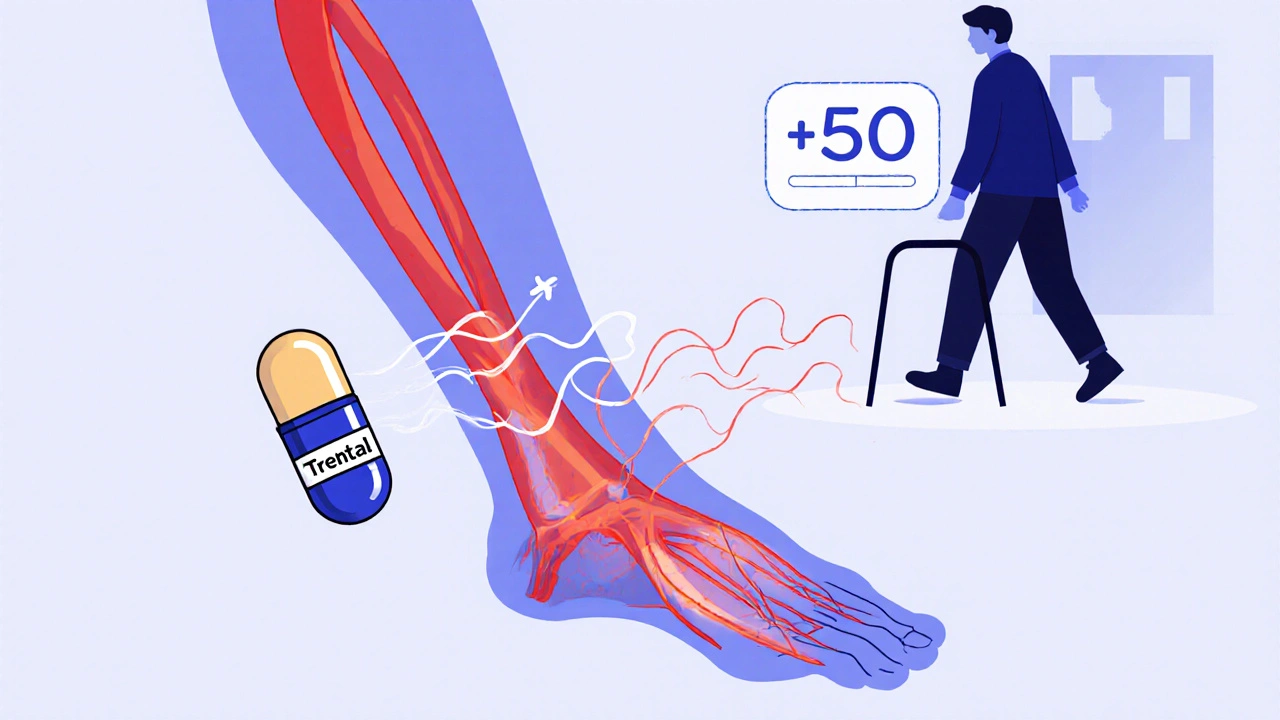
Trental (pentoxifylline) isn’t a household name, but for people with peripheral artery disease (PAD), it’s been a go-to option for decades. It’s not a miracle drug, but it helps improve blood flow in narrowed arteries - especially in the legs - reducing cramping and improving walking distance. Still, many patients and doctors are asking: Are there better options today? Is Trental still worth taking? Let’s cut through the noise and compare Trental with the most common alternatives, what they actually do, and who benefits most from each.
How Trental (Pentoxifylline) Works
Pentoxifylline, sold under the brand name Trental, is a hemorrheologic agent. That’s a fancy way of saying it makes blood less sticky and improves its ability to flow through small vessels. It works by reducing the thickness of blood, making red blood cells more flexible, and slightly widening blood vessels. This helps oxygen reach muscles in the legs that aren’t getting enough due to narrowed arteries.
It’s not a vasodilator like nitroglycerin. It doesn’t open arteries wide. Instead, it helps blood move more easily through already narrowed ones. Clinical trials show that Trental can increase walking distance by about 50 to 100 meters on average over 3 to 6 months. That’s not dramatic, but for someone who can only walk two blocks before leg pain forces them to stop, even 50 extra meters matters.
It’s taken orally, usually three times a day with meals. Common side effects include upset stomach, dizziness, and headaches. These are usually mild but can be enough to make people stop taking it. It also interacts with blood thinners like warfarin, so dosage adjustments are often needed.
Why People Look for Alternatives
Despite being approved by the FDA in the 1980s, Trental’s popularity has dropped. Why? Three big reasons:
- Modest results: The improvement in walking distance is small compared to newer options.
- Side effects: GI issues are common and can be hard to tolerate long-term.
- Lack of strong outcome data: Unlike statins or blood pressure meds, Trental hasn’t been shown to reduce heart attacks, strokes, or death.
Most patients today aren’t starting with Trental. Doctors often recommend lifestyle changes and other medications first. But if those don’t work, Trental is still in the toolbox - and so are its alternatives.
Alternative #1: Cilostazol (Pletal)
Cilostazol, sold as Pletal, is the most direct competitor to Trental. It’s also taken orally, twice a day, and targets the same problem: intermittent claudication from PAD.
But here’s the difference: Cilostazol works by blocking an enzyme that causes blood vessels to narrow and platelets to clump. This means it not only improves blood flow but also prevents clots. Studies show it increases walking distance by 100 to 150 meters on average - about twice the benefit of Trental.
Side effects? More than Trental. Diarrhea, headache, and palpitations are common. It’s also not safe for people with heart failure because it can increase heart rate. But for someone without heart issues, it’s often the first choice after lifestyle changes.
One big advantage: Cilostazol has been shown to reduce the need for vascular procedures like angioplasty over time. Trental hasn’t shown that benefit.
Alternative #2: Statins (Atorvastatin, Rosuvastatin)
Statins are cholesterol-lowering drugs, but their role in PAD goes way beyond lowering LDL. They reduce inflammation in artery walls, stabilize plaques, and improve endothelial function - the lining of blood vessels.
Large studies like the Heart Protection Study showed that statins reduce the risk of heart attack, stroke, and death in PAD patients by up to 25%. That’s huge. And while they don’t directly improve walking distance like Trental or Cilostazol, they stop the disease from getting worse.
Most guidelines now say: If you have PAD, you should be on a high-intensity statin - even if your cholesterol is normal. That’s not an alternative to Trental. It’s a foundation. Trental might help you walk farther today. Statins help you live longer and avoid amputation.

Alternative #3: Antiplatelets (Aspirin, Clopidogrel)
Because PAD is caused by atherosclerosis - a buildup of plaque - preventing clots is critical. That’s where antiplatelets come in.
Aspirin (81 mg daily) is the most common. It’s cheap, widely available, and reduces the risk of heart attack and stroke in PAD patients by about 20%. Clopidogrel (Plavix) is slightly more effective but more expensive. Some studies suggest clopidogrel works better than aspirin in PAD, especially in people who’ve had a prior event.
These drugs don’t improve walking distance. But they’re often prescribed alongside Trental or Cilostazol because they protect against the bigger dangers: heart attack and stroke.
Alternative #4: Lifestyle Changes - The Real Game-Changer
No medication works as well as walking. That’s not a joke. Supervised exercise therapy - walking until pain hits, resting, then repeating - has been shown to improve walking distance by 150 to 200 meters over 12 weeks. That’s better than Trental and close to Cilostazol.
It’s not glamorous. It’s not a pill. But it’s the most effective treatment for PAD that we have. Studies from the American Heart Association show that patients who stick with a 30-minute, 3-times-a-week walking program see long-term gains that last years.
Smoking cessation is even more important. If you smoke and have PAD, quitting is the single best thing you can do. It cuts your risk of amputation by 50% and improves survival more than any drug.
Alternative #5: Endovascular Procedures and Surgery
For severe PAD - where pain happens even at rest, or ulcers won’t heal - medications alone aren’t enough. That’s when doctors consider angioplasty, stenting, or bypass surgery.
These procedures physically open or reroute blocked arteries. They offer immediate relief. But they’re invasive, carry risks, and aren’t always long-lasting. Many patients need repeat procedures.
Medications like Trental or Cilostazol are often used before and after these procedures to improve healing and prevent re-blockage.
Comparison Table: Trental vs. Alternatives
| Medication/Approach | Improves Walking Distance | Reduces Heart Attack/Stroke Risk | Common Side Effects | Dosing |
|---|---|---|---|---|
| Trental (Pentoxifylline) | Yes (50-100 meters) | No | Upset stomach, dizziness, headache | Three times daily with meals |
| Cilostazol (Pletal) | Yes (100-150 meters) | Yes (indirectly) | Diarrhea, headache, palpitations | Twice daily, before meals |
| Statins (e.g., Atorvastatin) | No | Yes (up to 25% reduction) | Muscle pain, liver enzyme changes | Once daily, any time |
| Aspirin or Clopidogrel | No | Yes (20-25% reduction) | Bleeding risk, stomach irritation | Once daily |
| Supervised Exercise | Yes (150-200 meters) | Yes | Fatigue, muscle soreness | 30 min, 3x/week |

Who Should Take Trental Today?
Trental isn’t first-line anymore. But it still has a place:
- If you can’t take Cilostazol due to heart issues or severe side effects
- If you’re allergic to or can’t afford Cilostazol
- If you’ve tried statins and antiplatelets and still have symptoms
- If you’re not a candidate for exercise therapy (due to mobility issues or severe arthritis)
It’s also sometimes used in combination - for example, with aspirin and a statin - when symptoms persist.
What’s the Bottom Line?
There’s no single best drug for PAD. The most effective approach combines multiple strategies:
- Take a high-intensity statin every day
- Use aspirin or clopidogrel to prevent clots
- Start a supervised walking program - no excuses
- Quit smoking - if you smoke
- If symptoms persist, consider Cilostazol
- Trental? Only if nothing else works or isn’t tolerated
Trental helped many people walk farther in the past. But today, we have better tools. The goal isn’t just to relieve leg pain - it’s to keep you alive, mobile, and independent for decades to come.
Frequently Asked Questions
Is Trental still prescribed today?
Yes, but less often than before. Most doctors now start with statins, antiplatelets, and exercise. Trental is usually considered only if those don’t help enough or if patients can’t take Cilostazol due to heart problems or side effects.
Can I take Trental with blood pressure meds?
Generally, yes. Trental doesn’t interfere with most blood pressure medications like ACE inhibitors or beta-blockers. But it can increase the effect of blood thinners like warfarin, so your doctor will need to monitor your INR levels closely if you’re on both.
Does Trental cause weight gain?
No, Trental isn’t linked to weight gain. Some people report bloating or stomach discomfort, which might feel like weight gain, but there’s no evidence it affects metabolism or fat storage.
How long does it take for Trental to work?
It usually takes 4 to 8 weeks to notice any improvement in walking distance. Some people don’t feel changes until after 3 months. It’s not a quick fix. Patience and consistent dosing are key.
Are there natural alternatives to Trental?
There’s no herbal supplement proven to replace Trental. But lifestyle changes - especially walking, quitting smoking, and eating a heart-healthy diet - are more effective. Some studies show omega-3 fatty acids and beetroot juice may mildly improve circulation, but they’re not substitutes for prescribed treatment.
What happens if I stop taking Trental?
Symptoms like leg cramping during walking will likely return within a few weeks. Trental doesn’t change the underlying disease - it just helps blood flow better. Stopping it means losing that temporary benefit. Always talk to your doctor before discontinuing.
Next Steps
If you’re on Trental and wondering if you should switch:
- Ask your doctor about starting a statin if you’re not already on one.
- Find a cardiac rehab program near you for supervised walking therapy - Medicare often covers it.
- If you’re still having trouble walking after 3 months on Trental, ask about Cilostazol.
- If you smoke, make quitting your top priority. Your doctor can prescribe nicotine patches, varenicline, or refer you to counseling.
Peripheral artery disease isn’t just about leg pain. It’s a warning sign your whole vascular system is under stress. The best treatment isn’t a pill - it’s a plan. And that plan should include movement, medicine, and mindset.

Lexi Brinkley
November 8, 2025 AT 09:56Kelsey Veg
November 9, 2025 AT 03:09Alex Harrison
November 10, 2025 AT 11:33Jay Wallace
November 12, 2025 AT 03:38Alyssa Fisher
November 13, 2025 AT 22:28Alyssa Salazar
November 15, 2025 AT 01:13Beth Banham
November 16, 2025 AT 10:22Brierly Davis
November 17, 2025 AT 11:58Amber O'Sullivan
November 18, 2025 AT 17:38Jim Oliver
November 19, 2025 AT 07:01William Priest
November 21, 2025 AT 07:00Ryan Masuga
November 22, 2025 AT 19:45