QT Prolongation Risk Calculator
Understand Your Risk
This calculator estimates your QT interval prolongation risk when taking antipsychotics with other QT-prolonging medications. Risk increases dramatically when combining drugs that affect heart electrical activity.
Risk Assessment
When you take an antipsychotic for schizophrenia, bipolar disorder, or severe depression, your doctor focuses on calming your mind. But there’s another system in your body that’s quietly affected-your heart. Many of these medications don’t just alter brain chemistry; they also interfere with the heart’s electrical rhythm. When combined with other common drugs that do the same thing, the risk of a dangerous, sometimes deadly, heart rhythm problem called QT prolongation jumps dramatically.
What QT Prolongation Really Means
The QT interval is a measurement on an ECG that shows how long it takes your heart’s ventricles to recharge between beats. If this interval gets too long-over 450 ms in men, 460 ms in women-it creates a window where the heart can slip into a chaotic rhythm called torsades de pointes. This isn’t just a blip on a screen. It’s a type of ventricular arrhythmia that can lead to fainting, seizures, or sudden cardiac death.
This isn’t theoretical. Between 2010 and 2022, the FDA documented 128 cases of torsades de pointes linked to patients taking antipsychotics along with other QT-prolonging drugs. The risk doesn’t just add up-it multiplies. Studies show that when two QT-prolonging drugs are combined, the QT interval can stretch 2.3 to 4.7 times more than with either drug alone.
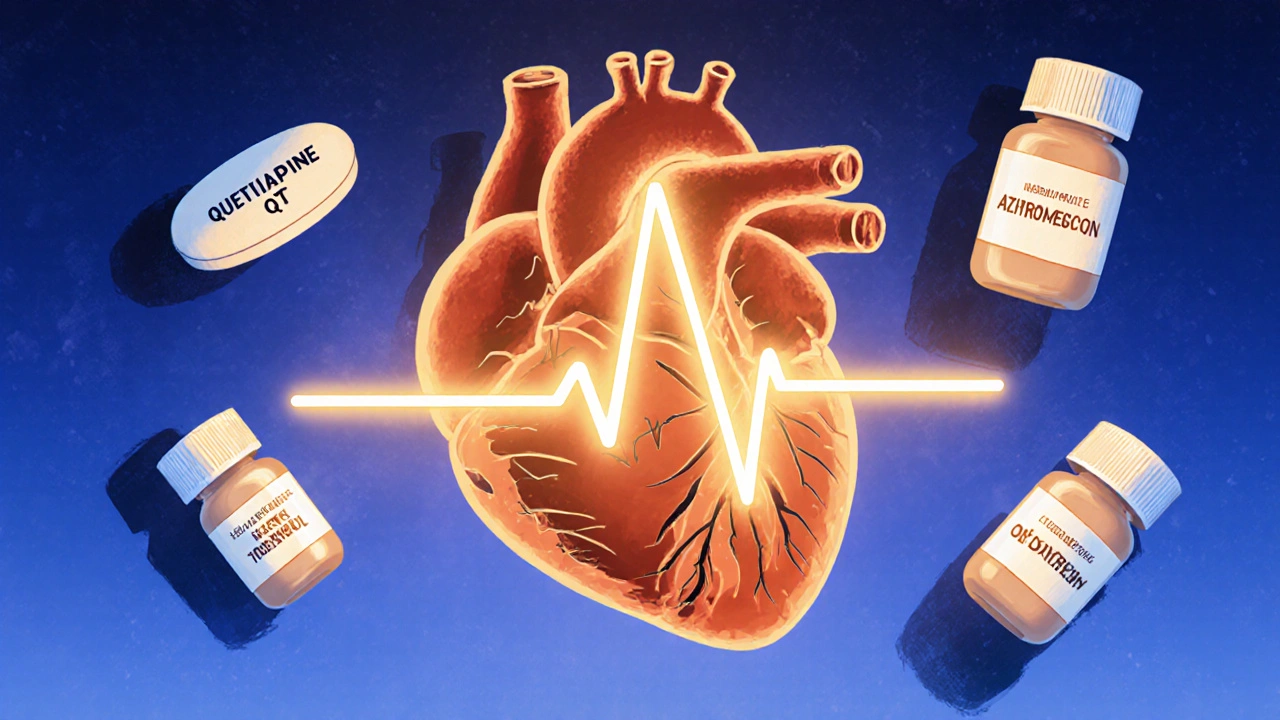
Which Antipsychotics Carry the Highest Risk?
Not all antipsychotics are created equal when it comes to heart safety. The risk depends on how strongly they block the hERG potassium channel, which controls the heart’s repolarization. Here’s how they break down:
- High-risk: Thioridazine (withdrawn in the U.S. but still used abroad), ziprasidone, haloperidol. These have IC50 values under 1 μM, meaning they’re very potent at blocking hERG.
- Moderate-risk: Quetiapine, risperidone, olanzapine. These are commonly prescribed and still carry real risk, especially in combination.
- Low-risk: Aripiprazole, brexpiprazole, lurasidone. These have IC50 values above 10 μM and show minimal QT prolongation in clinical studies.
Thioridazine was pulled from the U.S. market in 2005 because of its link to sudden death. Yet, quetiapine and risperidone-both moderate-risk-are still among the most prescribed antipsychotics in the country. In 2023, quetiapine was filled over 24 million times. That’s millions of people whose hearts are under subtle but real stress.
Other Drugs That Make Things Worse
It’s not just antipsychotics. Many other medications you might be taking can push your QT interval into danger territory:
- Antibiotics: Moxifloxacin, azithromycin
- Anti-nausea drugs: Ondansetron, promethazine
- Antiarrhythmics: Sotalol, amiodarone
- Antidepressants: Citalopram, escitalopram
A 2018 JAMA Internal Medicine study found that combining an antipsychotic with an antidepressant increased torsades risk by 4.3 times. Another study showed that adding ondansetron (a common anti-nausea drug) to an antipsychotic stretched the QT interval by nearly 39 milliseconds-far more than the antipsychotic alone.
And here’s the catch: 45% of people on antipsychotics are also taking at least one other QT-prolonging drug. Many patients don’t even know it. A nurse might give you ondansetron for chemo nausea. Your primary care doctor prescribes azithromycin for a sinus infection. Neither knows you’re on risperidone. That’s when the danger spikes.
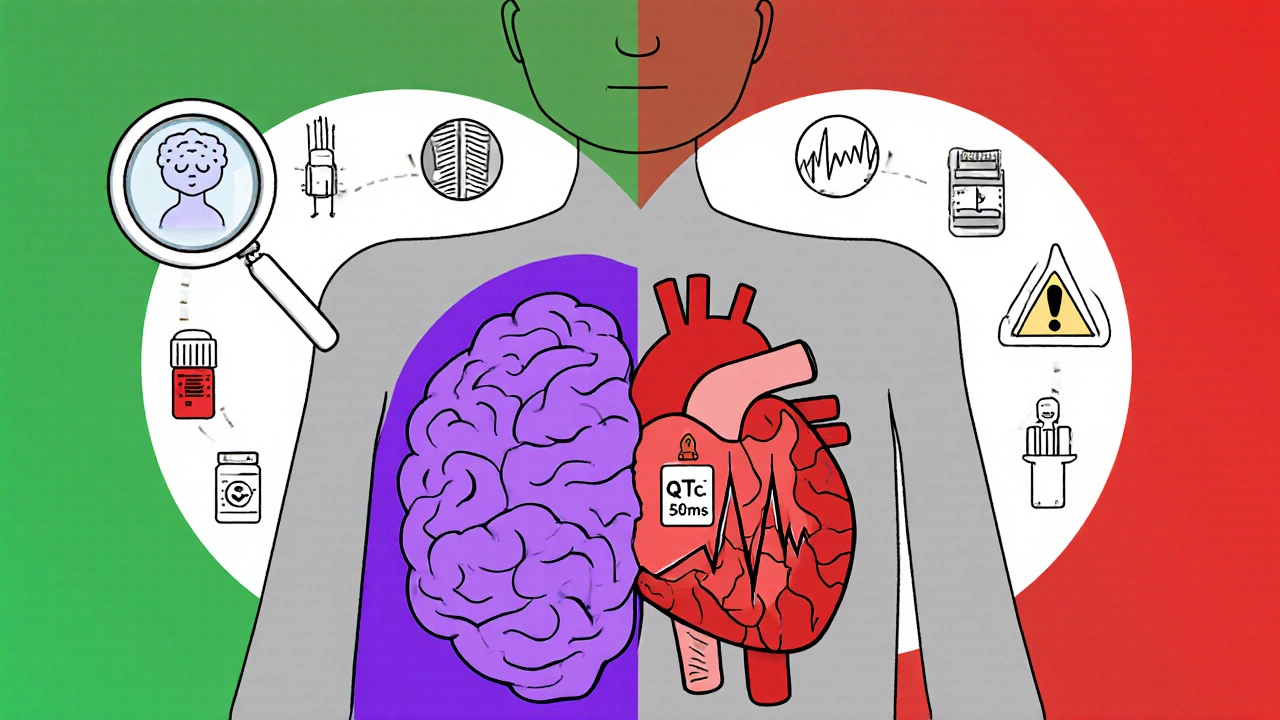
Who’s Most at Risk?
It’s not just the drugs-it’s you. Certain factors make QT prolongation more likely:
- Age over 65: Adds 15.3 ms to your QT interval
- Female sex: Adds 12.8 ms
- Low potassium (<3.5 mmol/L): Adds 22.7 ms
- Low magnesium: Also increases risk
- Slow heart rate (<50 bpm): Adds 18.4 ms
- Genetics: Poor metabolizers of CYP2D6 (7-10% of Caucasians) build up higher drug levels
Combine a 70-year-old woman on quetiapine with low potassium and a course of moxifloxacin? That’s a perfect storm. One case from Cleveland Clinic involved a 68-year-old woman whose QTc jumped from 448 ms to 582 ms in just 72 hours after starting ciprofloxacin. She nearly died.
How Doctors Should Monitor You
The American Heart Association and American Psychiatric Association agree: baseline ECG is essential. Here’s what they recommend:
- Get an ECG before starting a high- or moderate-risk antipsychotic.
- Repeat it within one week of starting.
- For high-risk combinations (antipsychotic + another QT drug), check ECG weekly for the first month, then monthly.
- For single moderate-risk drugs, check at 1 week, 4 weeks, then every 3 months.
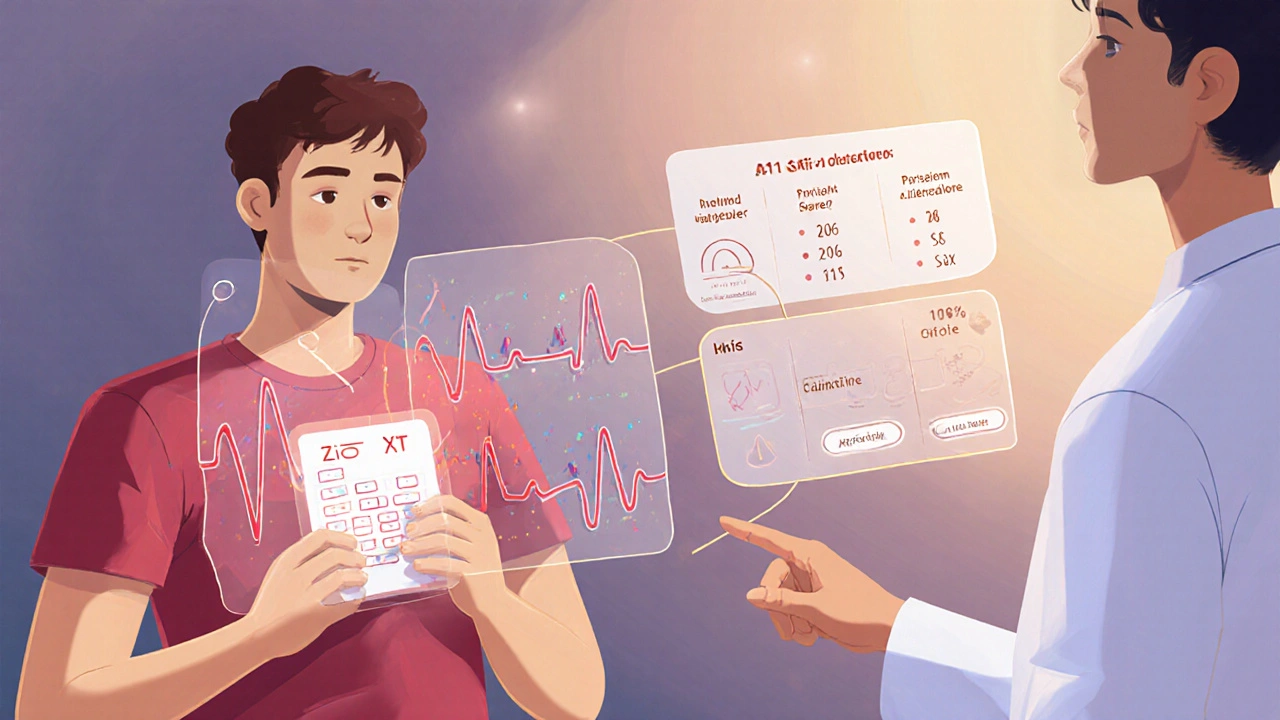
But here’s the problem: compliance is low. In community settings, fewer than 35% of patients get the recommended ECGs. Insurance often denies repeat ECGs. Rural clinics don’t have the equipment. A 2023 survey found 68% of clinicians reported insurance denials as a major barrier.
There’s a new tool changing this: the Zio XT patch. Approved by the FDA in May 2024, this wearable ECG patch can be worn for up to 14 days. It caught 98.7% of dangerous QTc spikes in a 2023 NEJM study. It’s not perfect-but it’s better than waiting for symptoms.
What You Can Do
If you’re on an antipsychotic, here’s what matters:
- Ask your doctor: Is my medication high-risk for QT prolongation? What’s my baseline QTc?
- Know your other meds: Make a list of every pill, including antibiotics and OTC drugs. Bring it to every appointment.
- Get your potassium checked: Low potassium is one of the most preventable triggers. A simple blood test can help.
- Don’t ignore symptoms: Dizziness, palpitations, fainting-don’t brush them off. They could be your heart warning you.
- Ask about alternatives: If you’re on risperidone or quetiapine and have other risk factors, ask if aripiprazole or lurasidone might be safer for you.
One patient on Reddit said she stopped her antipsychotic because she was terrified of her heart stopping. She wasn’t told the actual risk was less than 1 in 10,000 per year-unless she was on multiple drugs. That fear came from silence, not science.
The Bigger Picture
The market is shifting. Low-risk antipsychotics like aripiprazole are growing at 8.4% per year. By 2027, they’re projected to make up over half of new prescriptions. Why? Because regulators are pushing for change. The European Medicines Agency now requires drug labels to list exact combination risks. Medicare is starting to tie reimbursement to proper ECG monitoring.
Meanwhile, new tools are emerging. A 2025 guideline update will include a risk calculator that factors in age, sex, drug combinations, and electrolyte levels. In 2026, a genetic test will identify people who metabolize drugs slowly-helping doctors avoid dangerous doses before they’re even prescribed.
The goal isn’t to scare you off your medication. It’s to make sure you get the mental health care you need without putting your heart at unnecessary risk. With the right monitoring, the chance of torsades de pointes drops to less than 1 in 100,000 patient-years. That’s not zero-but it’s close enough to be safe.
Can antipsychotics cause sudden death?
Yes, but only under specific conditions. Most antipsychotics alone carry a very low risk of sudden cardiac death-about 1 in 25,000 patient-years. The real danger comes when they’re combined with other QT-prolonging drugs, especially in people with other risk factors like low potassium, older age, or female sex. In these cases, the risk can increase by 4 to 7 times. Sudden death from torsades de pointes is rare but preventable with proper monitoring.
Are there safer antipsychotics than quetiapine or risperidone?
Yes. Aripiprazole, brexpiprazole, and lurasidone have much lower hERG blockade activity and show minimal QT prolongation in clinical studies. Their risk of causing torsades de pointes is statistically similar to placebo. Many psychiatrists now start with these low-risk options, especially for patients with heart disease, older adults, or those already on other medications that affect the heart.
Do I need an ECG if I’m on a low-risk antipsychotic?
For most people on low-risk antipsychotics like aripiprazole or lurasidone, routine ECGs aren’t required unless you have other risk factors-like being over 65, having heart disease, or taking other QT-prolonging drugs. The American Heart Association doesn’t recommend routine monitoring for low-risk monotherapy. But if you’re on multiple medications or have electrolyte imbalances, an ECG is still a good idea.
Can I take azithromycin or ciprofloxacin if I’m on an antipsychotic?
It’s risky. Both azithromycin and ciprofloxacin are known to prolong the QT interval. Combining them with moderate- or high-risk antipsychotics like quetiapine, risperidone, or haloperidol can push your QTc into the danger zone. If you need an antibiotic, ask your doctor for one that doesn’t affect the heart, like amoxicillin or doxycycline. If you must take a QT-prolonging antibiotic, get an ECG before and after starting it.
Why do some doctors say QT prolongation isn’t a big deal?
Some experts argue that the FDA’s warnings overstate the risk, pointing to real-world data showing very low rates of torsades de pointes-even with QT-prolonging drugs. The absolute risk remains under 1% per year in psychiatric populations. But this doesn’t mean the risk is zero. The key is context: a 1% risk is acceptable for a life-threatening psychiatric condition-but not if it’s avoidable. The goal isn’t to ignore the risk-it’s to manage it smartly with monitoring, not fear.
What Comes Next
The future of psychiatric care is moving toward precision. Genetic testing will soon tell you if you’re a slow metabolizer of certain antipsychotics. Wearable ECG patches will catch dangerous changes before they become emergencies. Risk calculators will help doctors weigh drug combinations before they’re even prescribed.
But until then, the most powerful tool you have is information. Know your meds. Know your numbers. Ask questions. Your mental health matters-and so does your heart.

Jennifer Bedrosian
November 8, 2025 AT 09:11Lashonda Rene
November 8, 2025 AT 23:56Andy Slack
November 9, 2025 AT 02:23Rashmi Mohapatra
November 9, 2025 AT 13:21Abigail Chrisma
November 9, 2025 AT 14:40Ankit Yadav
November 11, 2025 AT 14:08Meghan Rose
November 12, 2025 AT 16:22Steve Phillips
November 12, 2025 AT 23:40Clyde Verdin Jr
November 14, 2025 AT 22:44Key Davis
November 16, 2025 AT 15:19Cris Ceceris
November 16, 2025 AT 22:32Brad Seymour
November 17, 2025 AT 15:41Malia Blom
November 18, 2025 AT 03:26Erika Puhan
November 18, 2025 AT 19:45Abigail Chrisma
November 20, 2025 AT 07:15