Osteoporosis Treatment During Pregnancy – Safe Options & Guidance
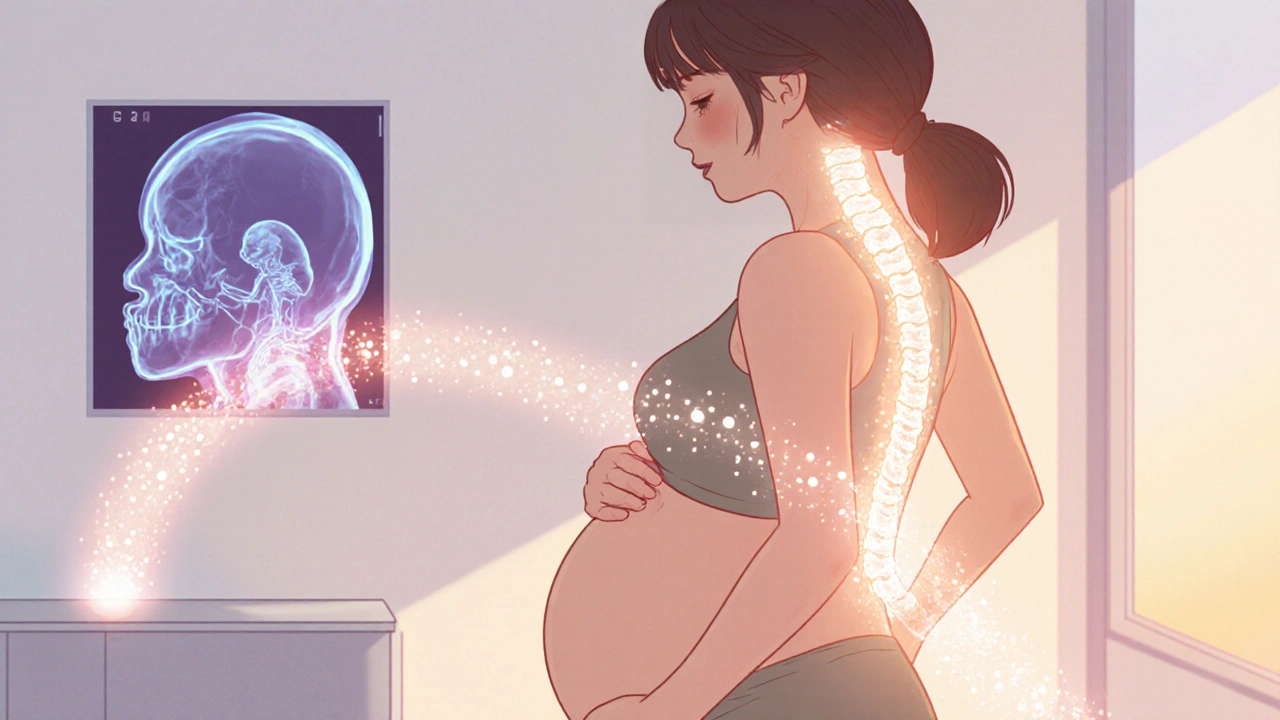
When it comes to osteoporosis treatment during pregnancy, managing bone loss while protecting the developing baby is the top priority. Also known as pregnancy‑safe osteoporosis care, it blends nutrition, gentle exercise, and careful drug choices to keep mom’s bones strong without risking fetal health.
One of the first pillars is calcium supplementation, a mineral that builds and maintains bone density. The body needs about 1,000 mg daily during pregnancy, and most prenatal vitamins fall short, so a dedicated calcium pill often fills the gap. Calcium works hand‑in‑hand with vitamin D, the sunshine‑derived vitamin that boosts calcium absorption. Without enough vitamin D, even a high calcium dose won’t stick to the bones.
Exercise isn’t a luxury; it’s a safe, drug‑free way to stimulate bone formation. Physical therapy, targeted low‑impact workouts like walking, swimming, and resistance bands, helps maintain bone density and improves balance, reducing fall risk. A qualified therapist can tailor a routine that respects the growing belly while still stressing the skeleton enough to keep it strong.
Key Considerations for Expectant Mothers
Medications that are mainstays for osteoporosis in non‑pregnant adults—such as bisphosphonates, drugs that slow bone breakdown—are generally off‑limits in pregnancy. Studies show they can cross the placenta and affect fetal bone development, so doctors avoid them unless the risk of fracture is life‑threatening. This creates a clear semantic link: osteoporosis treatment during pregnancy requires non‑pharmacologic strategies, while bisphosphonates are contraindicated. The same logic applies to newer agents like denosumab and selective estrogen modulators, which also lack safety data for the unborn child.
Because bone health is a cumulative process, early assessment matters. A simple dual‑energy X‑ray absorptiometry (DEXA) scan before conception or in the first trimester can flag severe loss, allowing clinicians to intervene with diet, supplements, and safe exercise plans. The goal is to keep the mother’s T‑score above the fracture‑risk threshold without introducing harmful substances.
Another important piece is overall nutrition. Adequate protein, magnesium, and vitamin K support bone matrix formation. Foods like leafy greens, dairy, fortified cereals, and legumes supply these nutrients naturally. When diet falls short, a prenatal multivitamin that includes the right amounts of calcium and vitamin D can bridge the gap without overdosing.
Finally, monitoring is essential. Regular blood tests for calcium, phosphorus, and vitamin D levels help fine‑tune supplementation. If levels drift, adjusting the dose is simple and keeps both mother and baby on track. This ongoing feedback loop illustrates another semantic triple: nutrient monitoring influences supplement dosage, which in turn maintains bone health during pregnancy.
Putting all these pieces together—nutrition, safe supplements, physical therapy, and careful avoidance of certain drugs—creates a comprehensive, pregnancy‑friendly approach to osteoporosis care. Below you’ll find a curated collection of articles that dig deeper into each of these topics, from the science behind calcium absorption to step‑by‑step exercise guides and the latest guidance on medication safety. Dive in to get the practical tips you need for a healthy pregnancy and strong bones.
Osteoporosis and Pregnancy: Essential Guide for Expectant Moms
- by Colin Edward Egan
- on 19 Oct 2025
Learn how pregnancy impacts bone health, identify risk factors, and discover safe nutrition, exercise, and medication tips to protect against osteoporosis.
