Glaucoma Treatment: What Works, What to Avoid, and How to Stay Ahead
When you hear glaucoma treatment, a medical approach to controlling eye pressure and preventing vision loss from optic nerve damage. Also known as pressure-lowering eye therapy, it’s not just about drops—it’s about stopping damage before you even notice it. Most people don’t feel glaucoma coming. No pain. No blurry vision at first. That’s why it’s called the silent thief of sight. By the time you see symptoms, the damage is often permanent. The goal of any real glaucoma treatment isn’t to cure it—it’s to stop it in its tracks.
At the heart of every effective plan is lowering intraocular pressure, the fluid pressure inside the eye that, when too high, crushes the optic nerve. This isn’t guesswork. Doctors measure it with a simple puff test. If it’s high, they start with eye drops—prostaglandins, beta-blockers, or carbonic anhydrase inhibitors. These aren’t just random meds; each one targets how fluid builds up or drains. Some increase outflow, others reduce production. You might need one, or a combo. And yes, they can cause side effects: red eyes, burning, even changes in heart rate or breathing. That’s why you can’t just pick one off the shelf. Your body’s response matters.
But pressure isn’t the only player. optic nerve damage, the irreversible harm caused by sustained high eye pressure, leading to blind spots and eventual vision loss can happen even when pressure looks normal. That’s why some patients need more than drops. Laser therapy can open drainage channels. Surgery might be needed if meds fail. And yes, genetics play a role too—just like with drug reactions in other areas of health. If someone in your family has glaucoma, you’re at higher risk. That’s not a scare tactic. It’s a signal to get checked early and often.
You’ll see posts here about how medications interact, how your genes affect drug response, and how even something as simple as timing your drops matters. One person’s miracle drop is another’s nightmare because of how their liver processes it. That’s why glaucoma treatment isn’t one-size-fits-all. It’s personal. It’s ongoing. And it’s not just about the eyes—it’s about protecting the rest of your life. Missing a dose? Forgetting to track pressure? These aren’t small slips. They add up.
Below, you’ll find real-world breakdowns of what works, what doesn’t, and how to avoid common mistakes. Some posts dig into drug interactions that could make your treatment less effective—or dangerous. Others show how genetic differences change how your body handles pressure-lowering meds. You’ll also see how lifestyle, timing, and even other health conditions tie into your eye health. This isn’t theory. It’s what people are actually using and learning from.
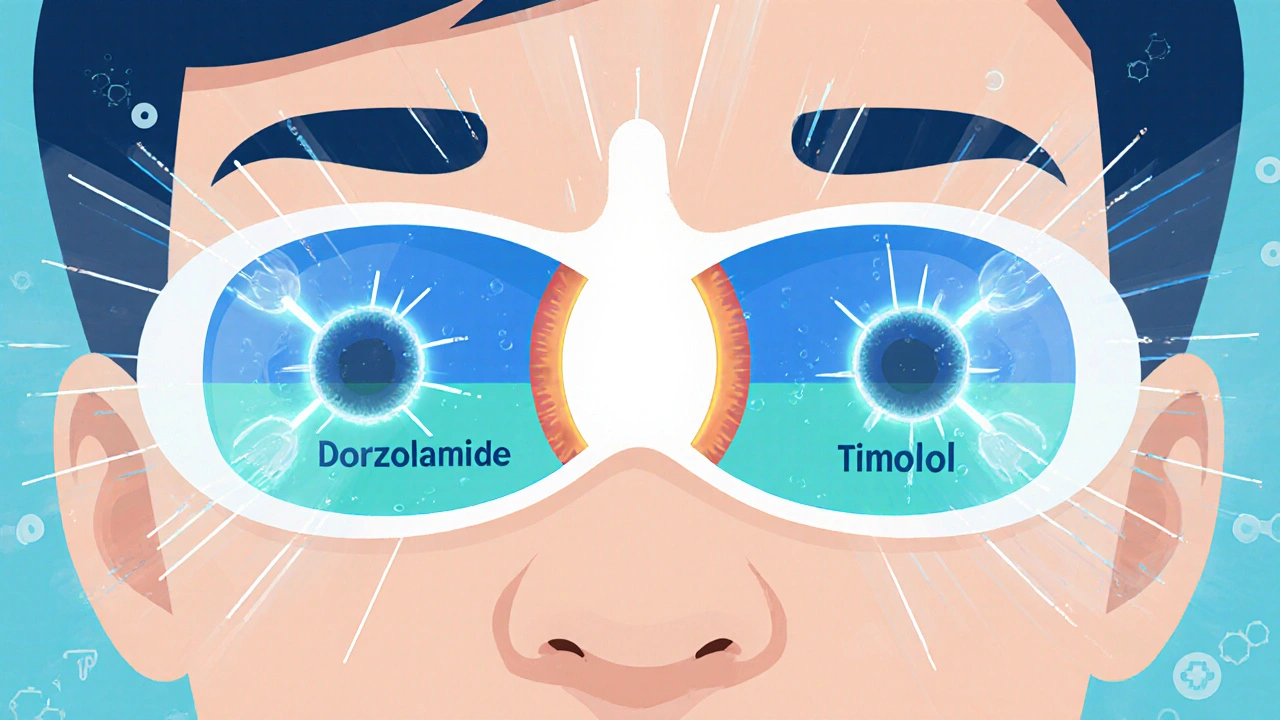
Dorzolamide-Timolol: The Ultimate Solution for High Eye Pressure
- by Colin Edward Egan
- on 31 Oct 2025
Dorzolamide-timolol is a two-in-one eye drop used to lower high eye pressure in people with glaucoma or ocular hypertension. It reduces fluid production in the eye and is effective, affordable, and widely prescribed. Learn how it works, its side effects, and how to use it correctly.
