If you’ve been told you have high eye pressure, you’re not alone. Millions of people in the U.S. are diagnosed with elevated intraocular pressure each year - and many of them are prescribed dorzolamide-timolol. It’s not a cure, but for a lot of people, it’s the difference between keeping their vision and losing it. This isn’t just another eye drop. It’s a two-in-one medication that tackles high eye pressure from two different angles. And if you’re wondering whether it’s right for you, here’s what actually matters.
What is dorzolamide-timolol?
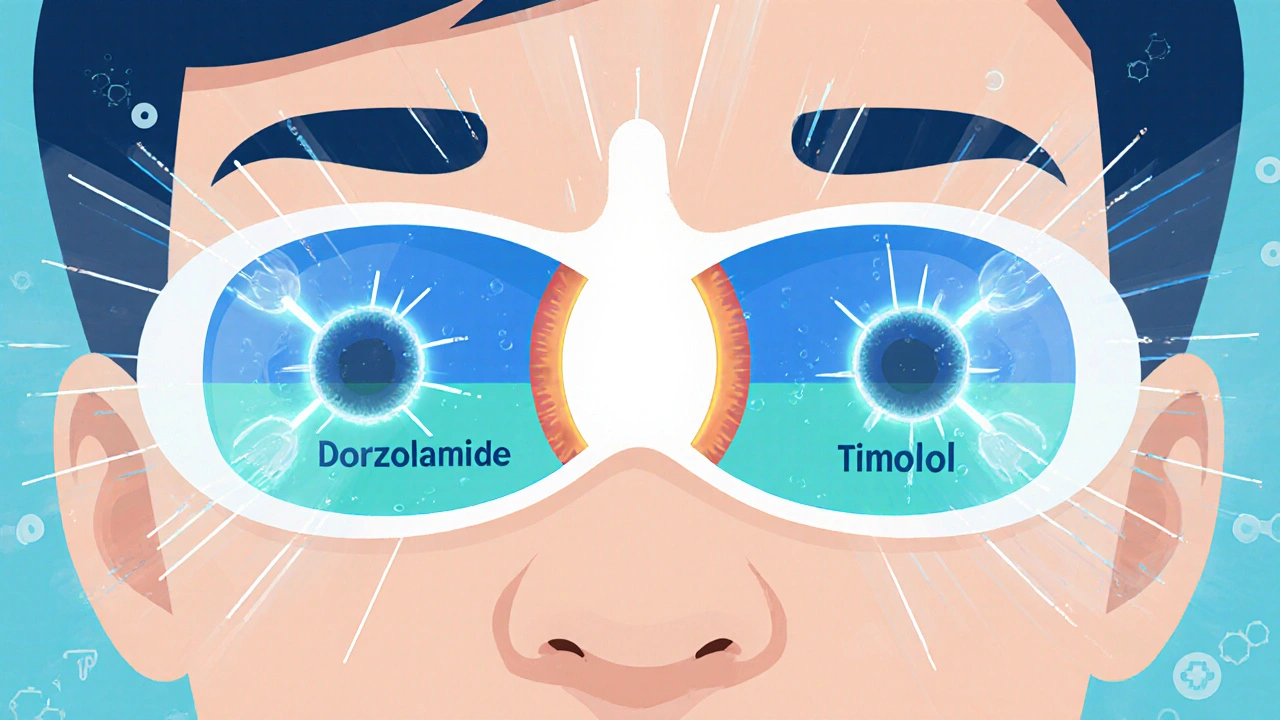
Dorzolamide-timolol is a combination eye drop that contains two active ingredients: dorzolamide is a carbonic anhydrase inhibitor, and timolol is a beta-blocker. They work together to reduce the amount of fluid inside your eye, which lowers pressure. High eye pressure, or intraocular pressure (IOP), is the main risk factor for glaucoma - a group of eye diseases that damage the optic nerve and can lead to permanent vision loss.
The brand name for this combination is Cosopt, but generic versions are widely available. Each milliliter of the solution contains 20 mg of dorzolamide and 5 mg of timolol. That’s the standard dose you’ll get unless your doctor adjusts it. It’s typically used twice a day - once in the morning and once in the evening. No more than that. More drops won’t lower pressure more, and they’ll just increase your risk of side effects.
How does it work?
Your eye constantly makes fluid - called aqueous humor - that nourishes the front part of the eye. Normally, this fluid drains out at the same rate it’s made. But in people with high eye pressure, the drainage system gets clogged or slows down. That causes fluid to build up, pushing against the optic nerve.
Dorzolamide works by reducing how much fluid your eye produces. It does this by blocking an enzyme called carbonic anhydrase, which is involved in fluid creation. Timolol does something similar but through a different pathway - it’s a beta-blocker that also cuts down fluid production. Together, they reduce fluid output by about 20-30%, which is enough to bring pressure down into a safer range for most people.
Unlike some other glaucoma medications, dorzolamide-timolol doesn’t improve drainage. It doesn’t open up the eye’s drainage channels. That’s important to know because if your drainage system is severely damaged, this medication alone might not be enough. That’s why doctors often pair it with other treatments.
Who benefits the most?
This combination isn’t for everyone. It’s most effective for people with open-angle glaucoma or ocular hypertension - the two most common causes of high eye pressure. Open-angle means the drainage angle of your eye is open but not working properly. Ocular hypertension means your pressure is high but you haven’t developed nerve damage yet.
It’s also commonly used when someone hasn’t responded well to single-agent drops. For example, if timolol alone lowered your pressure by 15% but you need 30%, adding dorzolamide can get you closer to your goal. Studies show that dorzolamide-timolol reduces eye pressure by an average of 25-30% compared to baseline, which is better than either drug alone.
It’s not recommended for people with certain heart conditions, asthma, or severe allergies to sulfa drugs (because dorzolamide contains a sulfa component). If you’ve had trouble with beta-blockers in the past - like slow heart rate or low blood pressure - your doctor will think twice before prescribing this.
What are the side effects?
Most people tolerate dorzolamide-timolol well. But side effects are common - and they’re often mild, but annoying. The most frequent ones include:
- Bitter taste in the mouth (yes, really - it happens because the drop drains into your nose and throat)
- Burning or stinging right after putting in the drop
- Red or itchy eyes
- Blurred vision for a few minutes
- Dry mouth or fatigue
Less common but more serious side effects include:
- Slow or irregular heartbeat
- Difficulty breathing (especially if you have asthma)
- Depression or mood changes
- Allergic reactions like swelling or rash
One thing patients often don’t realize: the bitter taste isn’t a sign the medicine isn’t working. It’s just how the ingredients travel. Swallowing a sip of water right after putting in the drop can help reduce it.

How to use it correctly
Using eye drops wrong is one of the biggest reasons they fail. If you’re not getting the full dose, your pressure won’t drop enough. Here’s how to do it right:
- Wash your hands.
- Tilt your head back and pull down your lower eyelid to form a pocket.
- Hold the bottle over your eye and squeeze one drop in - don’t let the tip touch your eye or eyelashes.
- Close your eye gently and press on the inner corner of your eye (near your nose) for one full minute. This blocks the tear duct and keeps the medicine in your eye longer.
- Wait at least five minutes before using another eye drop, if you’re on more than one.
Don’t skip doses. Missing even one or two doses a week can let pressure creep back up. Glaucoma doesn’t hurt. It doesn’t make your vision blurry right away. That’s why it’s called the "silent thief of sight." The damage happens slowly. You won’t notice until it’s too late.
How it compares to other treatments
| Medication | How It Works | Typical Pressure Reduction | Common Side Effects | Dosing Frequency |
|---|---|---|---|---|
| Dorzolamide-Timolol | Reduces fluid production (two mechanisms) | 25-30% | Bitter taste, burning, fatigue | Twice daily |
| Timolol alone | Reduces fluid production (beta-blocker) | 20-25% | Slow heart rate, breathing issues | Twice daily |
| Latanoprost | Increases fluid drainage | 25-33% | Darkened iris, eyelash growth | Once daily |
| Brimonidine | Reduces production + increases drainage | 20-28% | Dry mouth, drowsiness, allergic reactions | Three times daily |
| Combination: Brimonidine-Timolol | Same as above | 25-30% | Drowsiness, dry mouth | Twice daily |
Latanoprost is often the first choice because it only needs one drop a day and has fewer systemic side effects. But if you can’t use it - maybe because of cost, or because you’re pregnant, or because it causes your iris to darken - dorzolamide-timolol becomes a solid alternative. It’s also cheaper than some newer drugs.
Bruderine-timolol is another two-in-one option, but it causes more drowsiness and isn’t ideal if you drive a lot or work with machines. Dorzolamide-timolol doesn’t make you sleepy, which is a big plus for many people.
What if it doesn’t work?
Some people just don’t respond well. If your pressure stays above 18 mmHg after three months of using dorzolamide-timolol consistently, your doctor will likely switch or add another treatment. That could mean:
- Switching to latanoprost or another prostaglandin analog
- Adding a third medication like brimonidine or netarsudil
- Moving to laser treatment (SLT - selective laser trabeculoplasty)
- Considering surgery if pressure is dangerously high
Don’t wait. Glaucoma damage is irreversible. If your pressure isn’t controlled, your vision will slowly fade - starting with peripheral vision. You won’t notice until you’ve lost 40% of your sight. That’s why regular eye exams are non-negotiable.

Cost and accessibility
The brand-name Cosopt can cost over $200 without insurance. But the generic version? Around $30-$60 for a 5 mL bottle, depending on your pharmacy. Most insurance plans cover it. If you’re paying full price, check GoodRx or SingleCare - they often have coupons that bring the cost down to $15 or less.
It’s also available as a preservative-free version for people with sensitive eyes. That’s important if you’ve had irritation with other drops. The preservative benzalkonium chloride can cause long-term damage to the eye surface if used daily for years.
Long-term use and safety
People take dorzolamide-timolol for years - sometimes decades. Studies show it’s safe for long-term use. The main concern isn’t the medicine itself, but the fact that glaucoma keeps progressing. That’s why annual eye exams with an ophthalmologist are essential. They’ll check your optic nerve, your field of vision, and your pressure. No home test or phone app can replace that.
If you’re over 65, your doctor may monitor your heart rate and lung function more closely. Beta-blockers like timolol can affect breathing and heart rhythm in older adults. That’s not a reason to avoid it - just a reason to be monitored.
What you need to remember
- Dorzolamide-timolol is a two-drug combo that lowers eye pressure by reducing fluid production.
- It’s effective for open-angle glaucoma and ocular hypertension.
- Side effects are common but usually mild - bitter taste, burning, fatigue.
- It’s not a cure. It’s a tool to protect your vision.
- Use it exactly as prescribed. Missing doses risks permanent vision loss.
- It’s affordable as a generic, and most insurance covers it.
- If it doesn’t work after 3 months, talk to your doctor about alternatives.
High eye pressure doesn’t have to mean losing your sight. With the right treatment - and consistent use - dorzolamide-timolol can keep your pressure in check for years. But it only works if you use it. Not sometimes. Not when you remember. Every day, twice a day. That’s the deal.
Can dorzolamide-timolol cure glaucoma?
No. Dorzolamide-timolol doesn’t cure glaucoma. It only lowers eye pressure, which slows or stops the progression of nerve damage. Glaucoma is a lifelong condition that requires ongoing management. Stopping the drops can cause pressure to rise again and lead to vision loss.
Is it safe to use dorzolamide-timolol during pregnancy?
It’s not recommended. Timolol is a beta-blocker that can cross the placenta and affect the baby’s heart rate and growth. Dorzolamide is a sulfa drug, which also carries risks. If you’re pregnant or planning to be, talk to your eye doctor and OB-GYN about safer alternatives like latanoprost or laser treatment.
Can I use dorzolamide-timolol with contact lenses?
Remove your contacts before using the drops. Wait at least 15 minutes after putting in the drops before reinserting them. The preservatives in the solution can get trapped under the lenses and irritate your eyes. If you wear contacts daily, ask your doctor about preservative-free versions.
Why do I taste the medicine in my throat?
That’s normal. When you put in the drop, some of it drains through the tear duct into your nose and throat. That’s why you get a bitter taste. To reduce it, close your eye and press gently on the inner corner for one minute after applying the drop. This blocks the drainage pathway.
How long does it take for dorzolamide-timolol to work?
You’ll start to see pressure drop within a few hours of the first dose. But it takes about 2-4 weeks for the full effect to build. Don’t assume it’s not working if your pressure hasn’t dropped immediately. Stick with it, and your doctor will check your pressure after four weeks to see how you’re responding.
Can I stop using dorzolamide-timolol if my pressure seems normal?
Never stop without talking to your doctor. Even if your pressure seems normal, the underlying condition hasn’t gone away. Stopping the drops can cause pressure to spike again - sometimes dangerously high. Glaucoma damage is permanent and silent. You won’t feel it coming back until it’s too late.

Ravi Singhal
November 2, 2025 AT 00:20so i’ve been on this stuff for like 2 years now and honestly the bitter taste is the worst part lol. i just swallow a sip of water right after and it’s fine. also never thought about pressing the inner corner of my eye but wow that actually helps a ton. thanks for the tip!
Victoria Arnett
November 2, 2025 AT 00:45glad i found this i was about to switch to latanoprost but now i’m gonna stick with this since it’s cheaper and i dont get sleepy
HALEY BERGSTROM-BORINS
November 2, 2025 AT 23:19you know what they dont tell you… this stuff is part of a BIG PHARMA plot to keep you dependent. beta-blockers in your eyes?? what’s next? fluoride in the tears?? 🤔👁️💧
Sharon M Delgado
November 4, 2025 AT 14:02Oh, my goodness-this is so important! I cannot believe how many people just skip doses because they ‘feel fine’-but glaucoma doesn’t knock on your door, it sneaks in like a shadow, stealing your sight, one pixel at a time! Please, please, please-don’t be lazy with your drops! Your future self will thank you!
Dr. Marie White
November 6, 2025 AT 09:58I’ve seen patients struggle with this medication for years. The key isn’t just using it-it’s understanding why. Many think it’s a cure, not a shield. And the bitter taste? It’s not the medicine failing-it’s just the body’s way of saying, ‘Hey, this is going somewhere you didn’t expect.’
For those worried about side effects: talk to your doctor. Don’t assume it’s all in your head. And for those who think they’re fine because they don’t feel symptoms-glaucoma doesn’t scream. It whispers. And if you’re not listening, it’ll take everything.
Wendy Tharp
November 6, 2025 AT 13:03Why are we even using this? It’s just a Band-Aid on a bullet wound. Everyone’s just scared to admit that eye pressure meds are just profit machines. They don’t fix anything. They just keep you hooked. And don’t even get me started on the preservatives-those are slowly killing your corneas. But hey, at least you can afford it if you’re on Medicaid, right? 😏
Subham Das
November 8, 2025 AT 08:17One cannot help but reflect on the existential paradox of modern ophthalmology: we have the power to manipulate aqueous humor dynamics with exquisite precision, yet we remain utterly powerless against the metaphysical inevitability of entropy-of time, of decay, of the optic nerve’s quiet surrender. Dorzolamide-timolol is not medicine-it is a philosophical compromise. A temporary truce between the body and its slow unraveling. We are not curing glaucoma-we are merely delaying its poetry. And yet, we cling to these drops as if they were prayers written in chemical script.
Is it not ironic that the very enzyme we inhibit-carbonic anhydrase-is one that also regulates pH in our blood, our thoughts, our very breath? Are we not, in some metaphysical sense, silencing the voice of our own physiology? The bitter taste on the tongue-perhaps it is the flavor of hubris.
Cori Azbill
November 9, 2025 AT 10:22So let me get this straight-you’re telling me the government lets Big Pharma put beta-blockers in eye drops and we just accept it? And you think it's safe? What about all the veterans who got this prescribed and then had heart attacks? Coincidence? I think not. This is chemical warfare disguised as healthcare. And the fact that you’re not screaming about it means you’re part of the problem. 💥🇺🇸
Paul Orozco
November 9, 2025 AT 15:15Wait-you’re telling me this drops costs $30 generic? That’s insane. My cousin got it for $200 and she’s on Medicare. This system is rigged. You’re all just being manipulated. Why aren’t people talking about this? Why is no one holding the pharmacy chains accountable? This is a national scandal.
Bobby Marshall
November 10, 2025 AT 02:46Man, I used to hate these drops-burning, weird taste, felt like I was stabbing my eye with a tiny spoon. But after six months, I realized I could still see my grandkids’ faces clearly at bedtime. That’s worth a little sting. Seriously-don’t quit. It’s not glamorous, but it’s your vision. And that’s worth showing up for, every damn morning and night.
Ardith Franklin
November 10, 2025 AT 11:56They say it’s ‘safe for long-term use’-but who funded those studies? Who paid for the ‘research’? You think they’d publish data showing long-term corneal damage from benzalkonium chloride? Nah. They’d rather you go blind slowly than admit the preservative is toxic. This isn’t medicine-it’s a slow-motion cover-up.
Aneesh M Joseph
November 11, 2025 AT 07:10Why not just use one drop instead of two? You’re paying for two drugs but you only need one. This is just a scam to make you buy more. I stopped using it and my pressure didn’t change. So yeah, it’s fake.
Deon Mangan
November 12, 2025 AT 08:17Let me be the first to say this: you're doing an *excellent* job of preserving your ocular integrity. 🥂 Seriously, though-consistency is the unsung hero of glaucoma management. You're not just using drops-you're performing a daily act of rebellion against entropy. Keep going. And yes, the bitter taste? That's the flavor of vigilance. 🤓👁️
Vinicha Yustisie Rani
November 13, 2025 AT 08:32In my village, we say: the eye is the window to the soul, but only if you keep it clean and cared for. This medicine is not magic. It is discipline. Every drop is a promise you make to yourself-to see your children grow, to read the morning sun, to remember the faces you love. No pill, no drop, no doctor can do that for you. Only you can.