Drug-Induced Arrhythmia: Causes, Risks, and How to Stay Safe
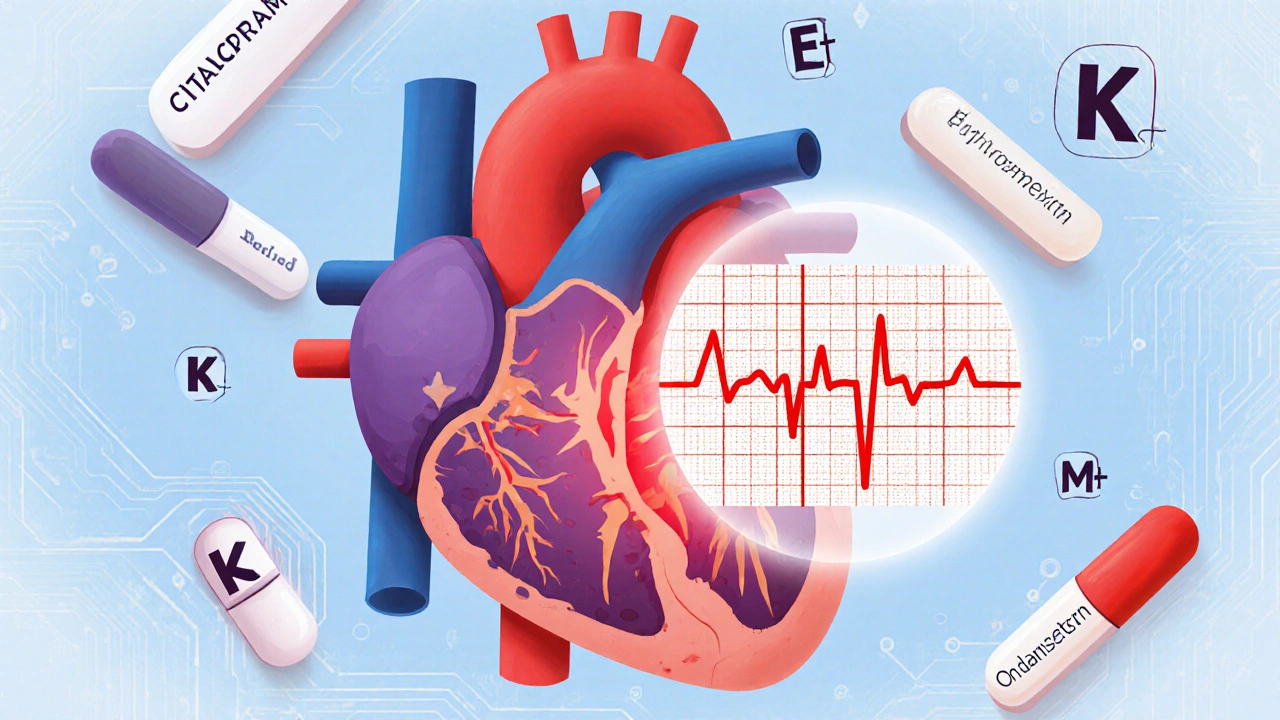
When a medication messes with your heart’s rhythm, it’s called drug-induced arrhythmia, an abnormal heartbeat triggered by drugs that interfere with the heart’s electrical signals. Also known as medication-related arrhythmia, this isn’t rare—it shows up in people taking everything from antibiotics to antidepressants, often without warning. Your heart beats because of tiny electrical pulses. Some drugs slow down, speed up, or scramble those signals. The result? A flutter, skip, or dangerous spike in heart rate that can lead to fainting, stroke, or even sudden death.
This isn’t just about one bad pill. It’s about combinations. QT prolongation, a delay in the heart’s electrical recovery phase, is the most common pathway to torsades de pointes. It’s the silent trigger behind many drug-induced arrhythmias. Drugs like certain antipsychotics, antibiotics, and even some antifungals can stretch that electrical cycle. When you add another QT-prolonging drug—say, an antidepressant on top of an antibiotic—the risk doesn’t just add up. It multiplies. And it’s not just the drugs themselves. Genetics play a role too. Some people have genes that make them extra sensitive. A dose that’s fine for one person could be deadly for another.
Medication interactions are the hidden danger here. You might be taking a safe dose of one drug, but throw in a new antibiotic, antifungal, or even a common supplement, and your heart’s rhythm can flip. This is why doctors check your full list of meds—not just the big ones. Even over-the-counter cold pills or herbal remedies can be risky if you’re already on something that affects your heart. And it’s not just older adults. Younger people with no history of heart problems are getting hit too, often because no one connected the dots between their new prescription and their racing heart.
It’s not all doom and gloom. The good news? This is preventable. If you’re on meds that affect your heart rhythm, your doctor can monitor you with an ECG. Blood tests can check for electrolyte imbalances—low potassium or magnesium—that make arrhythmias more likely. And if you feel dizzy, short of breath, or like your heart is skipping beats after starting a new drug, don’t wait. That’s not normal. That’s your body telling you something’s off.
Below, you’ll find real, practical guides from people who’ve been there. We’ve pulled together posts that break down exactly which drugs are most likely to cause trouble, how to spot the warning signs before it’s too late, and what to ask your doctor before you fill that next prescription. No fluff. Just what you need to protect your heart.
QT Prolongation and Sudden Cardiac Death from Medications: What You Need to Know About Risk Factors
- by Colin Edward Egan
- on 21 Nov 2025
QT prolongation from medications can lead to sudden cardiac death. Learn the key risk factors, which drugs are most dangerous, and how to protect yourself with simple checks and safer alternatives.
