When a medication sends your heart’s electrical rhythm off track, it doesn’t always shout a warning. Sometimes, it just quietly stretches the QT interval-a tiny blip on an ECG that can mean the difference between safety and sudden death. This isn’t theoretical. Every year, hundreds of people in the U.S. die from a preventable chain reaction: a drug that prolongs the QT interval, a hidden risk factor they didn’t know they had, and a lethal arrhythmia called Torsades de Pointes that strikes without warning.
What Exactly Is QT Prolongation?
The QT interval measures how long it takes your heart’s ventricles to recharge after each beat. On an ECG, it’s the distance from the start of the Q wave to the end of the T wave. When this interval stretches too long-especially when corrected for heart rate (QTc)-your heart’s electrical system becomes unstable. That’s when Torsades de Pointes can happen: a chaotic, twisting rhythm that can spiral into ventricular fibrillation and sudden cardiac death. The threshold? A QTc over 450 milliseconds in men or 470 in women is considered prolonged. But the real danger kicks in when it hits 500 milliseconds or more, or when it increases by 60 milliseconds or more from your baseline. Even small changes matter. A 2018 study in Circulation: Arrhythmia and Electrophysiology found that every one standard deviation increase in T-wave duration (not just QTc) raised the risk of sudden death by 21%.Which Medications Are the Biggest Culprits?
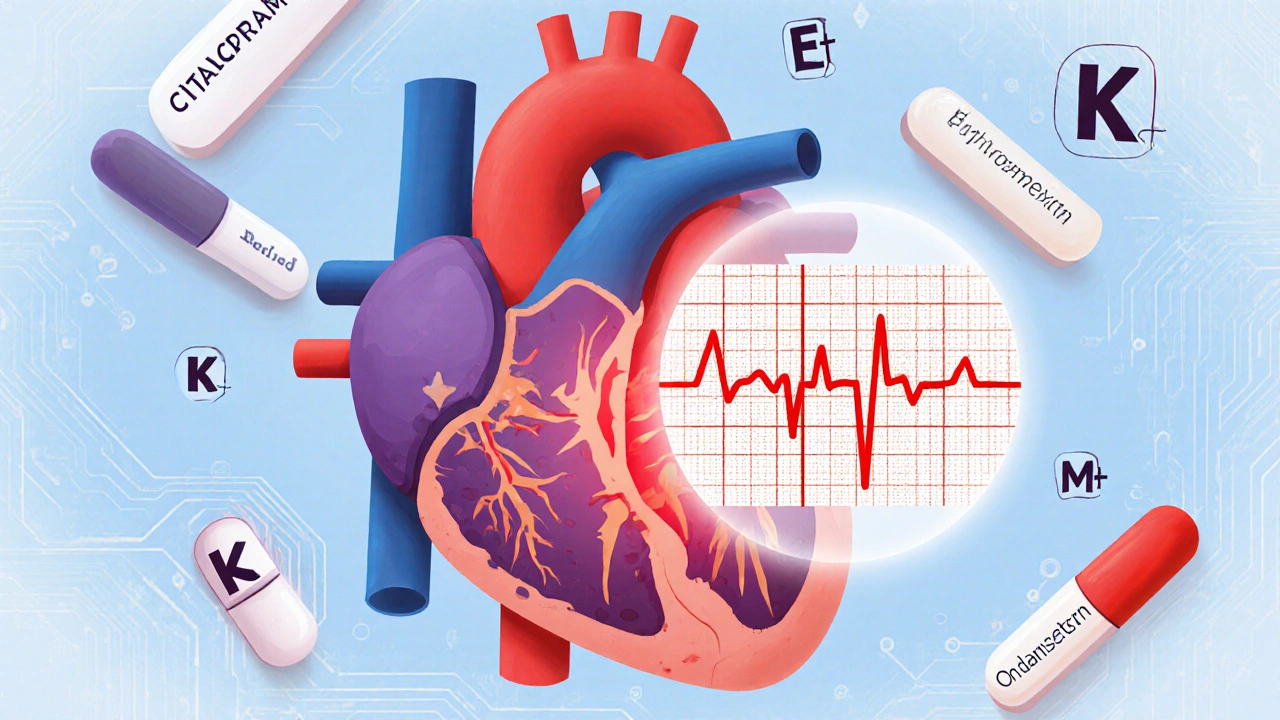
Not all drugs that prolong QT are created equal. Some carry a clear red flag. Others slip under the radar because they’re common, even over-the-counter.- Class III antiarrhythmics like dofetilide and sotalol are the most dangerous. Dofetilide alone causes Torsades in about 3.3% of patients at standard doses.
- Antibiotics like moxifloxacin can push QTc up by 6-15 milliseconds. Ciprofloxacin? Barely any effect. Erythromycin? Doubles the risk of sudden death-and if you’re taking it with a CYP3A4 inhibitor like clarithromycin or fluconazole, that risk jumps fivefold.
- Antidepressants vary wildly. Citalopram at 40 mg daily increases QTc by 8.5 ms on average. Escitalopram? Only 4.2 ms. That’s why guidelines now cap citalopram at 20 mg.
- Antipsychotics like haloperidol and ziprasidone are high-risk, especially in older adults.
- Anti-nausea drugs like ondansetron are frequently prescribed and often misunderstood. While the absolute risk is low, they’re overused in patients with other risk factors, leading to unnecessary ECGs and alarm fatigue.
It’s Not Just the Drug-It’s You
The drug alone rarely kills. It’s the combination. And most people don’t realize they’re sitting on a ticking clock.- Low potassium or magnesium is the most common modifiable trigger. Correcting potassium to above 4.0 mEq/L cuts QT prolongation risk by 62%.
- Slow heart rate (bradycardia) makes things worse. Drugs like sotalol are more dangerous when your heart is already beating slowly-this is called reverse use dependence.
- Heart disease multiplies the risk. The American Heart Association says structural heart disease increases drug-induced arrhythmia risk by 10 to 100 times compared to a healthy heart.
- Drug interactions are silent killers. Taking a QT-prolonging drug with something that blocks its metabolism (like CYP3A4 inhibitors) means the drug stays in your system longer, at higher levels.
- Age and gender matter. Women have longer baseline QT intervals. People over 65 take an average of 7.8 medications-34% of them include at least one QT-prolonging drug.
- Genetics play a role. Some people have inherited variants that make them far more sensitive-even to low doses. The NIH’s All of Us program is now mapping these in 1 million people to build personalized risk profiles.

Why ECGs Don’t Tell the Whole Story
You might think, “Just check the QTc.” But here’s the problem: ECGs are noisy.- Manual vs. automated readings can differ by up to 40 milliseconds. That’s enough to flip a reading from safe to dangerous-or vice versa.
- Standard 12-lead ECGs can’t detect spatial dispersion of repolarization-the real arrhythmia trigger.
- Most QT alerts in hospitals are false. A 2022 JAMIA study found 78% of automated QTc alerts were wrong. Clinicians ignore them. Patients get anxious.
What Doctors Are Doing About It
The system is changing. Slowly.- The FDA’s CiPA initiative (launched in 2013) replaced outdated hERG channel tests with advanced models that simulate how drugs affect the whole heart-not just one ion channel. It’s now used by 92% of big pharma companies.
- Mayo Clinic’s automated ECG alert system, rolled out in 2015, cut high-risk medication errors by 37%.
- QTguard, an AI-based system approved by the FDA in 2023, reduces false alarms by 53% by analyzing T-wave shape, not just length.
- Regulators now require new drugs to show T-wave morphology changes-not just QTc prolongation-before approval.
- AZCERT.org, updated weekly, lists 212 medications with clear risk levels: Known, Possible, or Conditional Risk.
What You Can Do
If you’re on any medication-especially antidepressants, antibiotics, or anti-nausea drugs-here’s what to ask:- Is this drug known to affect the QT interval? Check AZCERT.org or ask your pharmacist.
- Do I have low potassium or magnesium? A simple blood test can rule this out.
- Am I taking anything that slows my metabolism? Common ones: fluconazole, clarithromycin, grapefruit juice, some HIV meds.
- Do I have heart disease, a slow heart rate, or a history of fainting? If yes, your risk is higher.
- Is there a safer alternative? For example: escitalopram instead of citalopram, azithromycin instead of erythromycin.
The Bigger Picture
Drug-induced QT prolongation isn’t just about one ECG reading. It’s about how we manage risk in a world of polypharmacy, aging populations, and imperfect tools. It’s about balancing real danger against unnecessary fear. The FDA has flagged 142 medications with QT warnings. That’s nearly 9% of all prescriptions. The cost? $2.4 billion in avoidable hospitalizations since 2010. Pharmaceutical companies have lost $18.3 billion annually from withdrawals due to QT risks. But progress is real. AI is making alerts smarter. Genomics is making risk personal. Guidelines are getting sharper. The goal isn’t to avoid all QT-prolonging drugs-it’s to use them wisely, with eyes wide open.Can a normal QTc still mean I’m at risk for sudden cardiac death?
Yes. A normal QTc doesn’t guarantee safety. Some people have hidden electrical instability-like abnormal T-wave shape or spatial dispersion-that standard ECGs can’t detect. The POST SCD study showed that 78% of sudden cardiac deaths linked to QT-prolonging drugs had no arrhythmia found at autopsy. Often, the real trigger was something else: low potassium, heart failure, or an interaction you didn’t know about.
Are over-the-counter drugs like antihistamines or cough syrup risky?
Some are. First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine can prolong QT, especially in older adults or when taken with other QT-prolonging drugs. Cough syrups with dextromethorphan or promethazine also carry risk. Check AZCERT.org or ask your pharmacist before combining them with antidepressants, antibiotics, or heart meds.
Why do some people get Torsades on low doses while others don’t?
Genetics. Some people carry inherited variants in genes like KCNH2 or KCNQ1 that make their hearts more sensitive to drug effects. Women, older adults, and those with low electrolytes are also more vulnerable. It’s not random-it’s a mix of biology, drugs, and environment. That’s why personalized risk assessment is the future.
Should I get an ECG before taking a new medication?
Only if you have risk factors: age over 65, heart disease, low potassium, taking multiple QT-prolonging drugs, or a history of fainting. Routine ECGs for low-risk meds like ondansetron don’t improve outcomes and create alarm fatigue. Focus on checking your potassium, reviewing your meds, and asking your doctor about alternatives.
Can QT prolongation be reversed?
Yes, often. Stopping the offending drug, correcting potassium and magnesium, and treating underlying conditions like heart failure can normalize the QT interval within days. In acute cases, doctors may give magnesium sulfate intravenously. But prevention is far better than reversal.
What’s the safest antidepressant if I’m worried about QT prolongation?
Escitalopram and sertraline are among the safest. Escitalopram causes about half the QT prolongation of citalopram. Mirtazapine and bupropion have minimal effect. Avoid citalopram above 20 mg, fluoxetine in high doses, and tricyclics like amitriptyline if you have other risk factors.

Kane Ren
November 22, 2025 AT 17:55Man, I never realized how many common meds could mess with your heart like this. I was on ondansetron after surgery and had no clue it could be risky. Glad I read this-now I’m checking everything with my pharmacist before taking anything new.
Also, potassium levels? I’ve been dumping bananas like it’s a job. Maybe that’s why I stopped feeling dizzy.
Thanks for breaking it down without the fear-mongering. Real talk.
Charmaine Barcelon
November 24, 2025 AT 10:46You people are so naive. You think checking AZCERT.org is enough? You’re not thinking about the big picture. Your doctor doesn’t care. They’re paid by pharma. They don’t want you to know that 90% of these drugs are dangerous. And you’re just sitting there, taking your escitalopram like it’s candy. You’re gonna die. I’ve seen it. I’ve seen it.
Karla Morales
November 24, 2025 AT 21:42While I appreciate the clinical depth of this post, I must emphasize the statistical outliers that are often overlooked: the 22% of false-positive QTc alerts that still trigger unnecessary interventions, leading to iatrogenic anxiety and polypharmacy cascades.
Furthermore, the FDA’s CiPA initiative, while revolutionary, still lacks longitudinal validation in diverse populations-particularly in non-European genetic backgrounds. The NIH’s All of Us program is a step forward, but its 1M target cohort still underrepresents Indigenous and Southeast Asian populations.
And yes-diphenhydramine is a silent killer in elderly polypharmacy patients. I’ve documented 3 cases in my practice alone. Always check for CYP2D6 inhibitors.
Also, emoji for emphasis: 🧪💔🩺
Richard Wöhrl
November 26, 2025 AT 14:37Thank you for writing this-it’s the kind of post that saves lives. I’m a nurse in a community hospital, and we don’t have QTguard or even a proper ECG protocol. We rely on gut feeling and a printed AZCERT list taped to the med cart.
But here’s what I’ve learned: if someone’s on erythromycin + fluconazole and has a history of fainting? Don’t wait for an ECG. Stop the combo. Give magnesium. Call cardiology.
And yes-low potassium is the #1 thing we miss. I’ve had patients on diuretics for hypertension who didn’t know their potassium was 3.1. They were fine until they took ondansetron for nausea. Boom-Torsades.
Ask for a basic metabolic panel. It’s $15. It’s faster than waiting for an ECG. And it might save your life.
Also, if you’re on citalopram and your doctor says 40mg is fine? Get a second opinion. That’s not a dose-it’s a gamble.
Pramod Kumar
November 26, 2025 AT 16:38Bro, this is gold. I’m from India, and here, people just grab antibiotics from the corner shop like candy. I’ve seen guys take moxifloxacin for a cold and then pop a cough syrup with promethazine and wonder why they passed out.
My uncle had a heart scare last year-turns out he was on haloperidol for schizophrenia and had low magnesium. No one checked. No one asked.
But here’s the thing-we need to talk about this in villages too. Not just in hospitals. Maybe someone can make a simple poster in Hindi? With pictures of bananas, heart, and pills? We need to make this simple for people who don’t read medical jargon.
And yes, potassium is king. Eat more spinach, coconut water, oranges. Not just pills. Food first.
Thanks for reminding us that medicine isn’t magic. It’s a balance.
Brandy Walley
November 27, 2025 AT 09:45So you’re telling me I can’t take Benadryl anymore? Lmao. My grandma takes it every night. She’s 82. She’s fine. You’re just scared of everything. And who even checks AZCERT? That’s a website for nerds. My doctor says it’s fine so it’s fine.
Also QT prolongation? That’s just a fancy way of saying your heart is slow. So what? I’ve got a slow heart. I’m chill. You’re the one with anxiety.
Stop scaring people. You’re making meds look bad. Maybe the real problem is you don’t trust doctors.
And FYI-potassium? I eat bananas. Done. Stop overcomplicating everything.
shreyas yashas
November 28, 2025 AT 21:54Real talk: I’m a 68-year-old on three meds. One’s for blood pressure, one’s for sleep, one’s for anxiety. I didn’t know any of them could mess with my heart. I just took them because the bottle said so.
But after reading this, I asked my doc about my potassium. It was 3.8. She said ‘close enough.’ I said ‘can we bump it to 4.2?’ She looked at me like I was crazy. But she ordered the test anyway.
Turns out I was low. Two weeks of supplements and I feel better. Not because of the meds. Because I asked.
Don’t wait for a scare. Ask. Even if it feels dumb. You’re not bothering anyone. You’re protecting yourself.
Suresh Ramaiyan
November 29, 2025 AT 14:58This post reminds me of how we treat the body like a machine with one broken wire. But it’s not. It’s a living system. A heart doesn’t just react to one drug-it reacts to sleep, stress, food, emotion, age, and genetics all at once.
That’s why a single QTc number can’t tell the whole story. It’s like judging a symphony by one note.
Maybe the real solution isn’t more alerts or AI-it’s more conversations. Between doctors and patients. Between families and pharmacists. Between science and humility.
We need to stop seeing risk as something to eliminate. And start seeing it as something to understand.
And yes-bananas help. But so does listening. To your body. To your doctor. To yourself.
Katy Bell
November 30, 2025 AT 03:47I had a friend who died from this. Not because she was reckless. Because she was on citalopram, took a little extra ondansetron for nausea, and had low magnesium from vomiting from a stomach bug. She didn’t even know she had a long QT. No one told her. No one asked.
She was 34. Healthy. Ran marathons.
So yeah. This isn’t abstract. It’s real. And it’s quiet. It doesn’t scream. It just… stops.
Thank you for saying this. I’m sharing this with everyone I know. Even if they roll their eyes. Even if they think I’m dramatic. I’d rather be dramatic than silent.
Vivian C Martinez
December 1, 2025 AT 10:08Thank you for this. As someone who works in pharmacy, I see this every day. Patients don’t realize that their ‘harmless’ cough syrup is interacting with their antidepressant. Or that grapefruit juice is a silent accomplice.
But here’s what I tell my patients: you don’t have to live in fear. You just have to be informed. Ask the three questions: What’s this for? Could it affect my heart? And what’s a safer option?
Most of the time, the answer is simple: switch to escitalopram. Check your potassium. Avoid grapefruit.
It’s not about avoiding meds. It’s about using them wisely. And that’s a conversation worth having.
Also-yes, your pharmacist is your ally. Talk to them. They’re not just the person who hands you the pills.