PPI-Clopidogrel Effectiveness Calculator
This tool shows how different proton pump inhibitors (PPIs) affect clopidogrel's effectiveness based on clinical evidence. Clopidogrel is a crucial blood thinner after heart attacks or stent placement, but some PPIs can significantly reduce its effectiveness.
When you’re on clopidogrel after a heart attack or stent placement, your doctor prescribes it to keep your blood from clotting. But if you also have stomach issues - and many do - you might be told to take a proton pump inhibitor (PPI) like omeprazole to prevent ulcers. Sounds simple, right? Here’s the problem: omeprazole can seriously weaken clopidogrel’s ability to do its job. This isn’t theoretical. It’s happened in real patients. And the difference between a safe choice and a risky one can come down to which PPI you pick.
How Clopidogrel Actually Works (It’s Not What You Think)
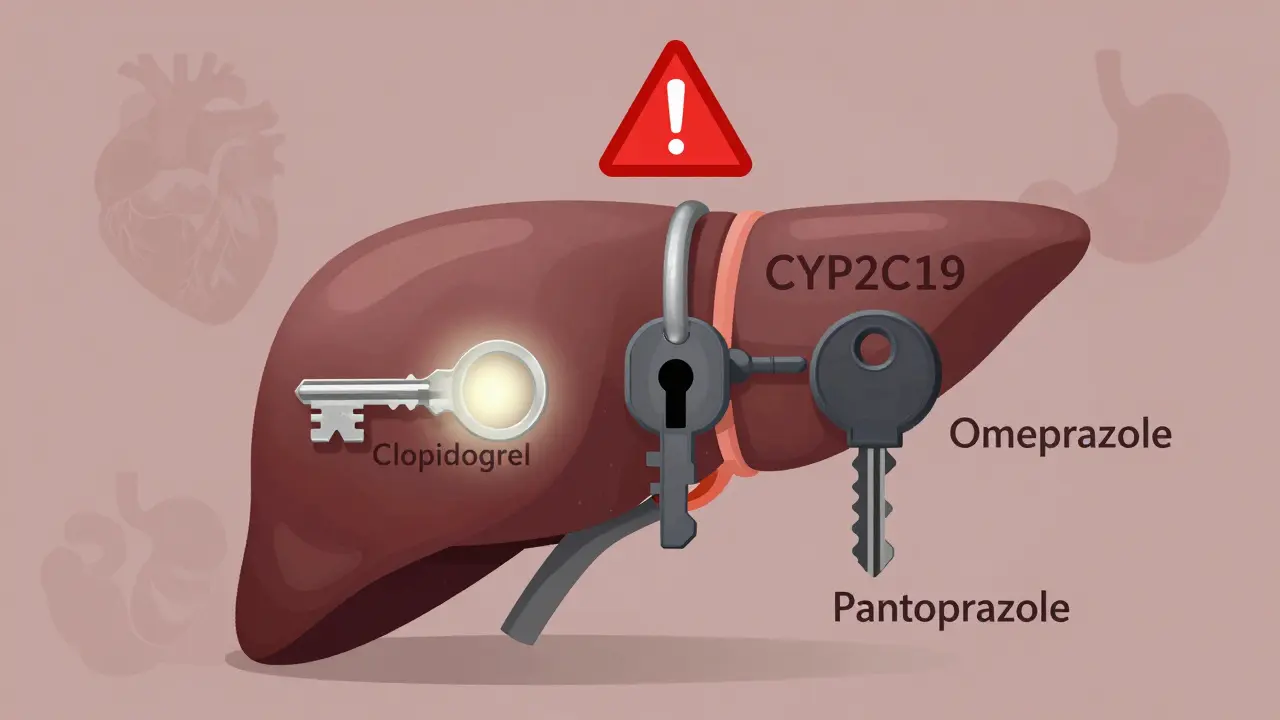
Clopidogrel isn’t active when you swallow the pill. It’s a pro-drug, meaning your liver has to turn it into something else before it works. That something else is a thiol metabolite that blocks platelets from clumping together. The enzyme responsible for this critical first step? CYP2C19. If this enzyme doesn’t do its job, clopidogrel doesn’t work - and your risk of another heart attack or stent clot goes up.
Here’s the twist: about 30% of people in the U.S. have a genetic variation that already makes CYP2C19 less effective. These are called loss-of-function alleles, mostly the *2 variant. People with this don’t activate clopidogrel well to begin with. They’re already at higher risk. Now, add a PPI that blocks CYP2C19, and you’re stacking the deck against the drug.
The PPI That Breaks Clopidogrel - Omeprazole
Not all PPIs are created equal. Omeprazole and its close cousin esomeprazole are the worst offenders. They bind tightly to CYP2C19, like a key that fits perfectly into the wrong lock. Studies show that even at standard doses (20mg daily), omeprazole cuts the amount of active clopidogrel metabolite in your blood by about 32%. At higher doses, it’s nearly half. That’s not a small drop - that’s enough to make the drug ineffective in many patients.
The FDA noticed this. In 2014, they updated clopidogrel’s label with a black box warning - the strongest kind - saying to avoid omeprazole and esomeprazole together. Why? Because multiple studies linked the combo to higher rates of heart attacks, stent clots, and even death. One landmark study found a 27% increase in cardiovascular events when clopidogrel was taken with omeprazole.
Why Pantoprazole Is the Safer Bet
Enter pantoprazole. Unlike omeprazole, it barely touches CYP2C19. It’s metabolized mostly through other liver pathways. Studies show it reduces clopidogrel’s effectiveness by only 14% - even at double the normal dose. In fact, a 2024 study in JAMA Network Open found pantoprazole had no significant effect on clopidogrel’s action at all.
The data doesn’t lie. A 2017 meta-analysis of 12 trials found omeprazole reduced clopidogrel’s antiplatelet effect by 38.5%. Pantoprazole? Just 3.7% - and that wasn’t even statistically meaningful. The COGENT trial, which looked at real-world outcomes, found no increase in heart events with pantoprazole, even while cutting GI bleeds by half.
That’s why top guidelines now say: if you need a PPI with clopidogrel, use pantoprazole or dexlansoprazole. The American College of Cardiology and the European Society of Cardiology both recommend avoiding omeprazole and esomeprazole entirely in these patients.
What About Rabeprazole and Lansoprazole?
Rabeprazole is a middle ground. It’s not as strong as omeprazole at blocking CYP2C19, but it still has some effect - about a 28% drop in peak metabolite levels. It’s better than omeprazole, but not as safe as pantoprazole.
Lansoprazole? It’s moderate. It inhibits CYP2C19 more than pantoprazole but less than omeprazole. If you’re stuck with it, don’t panic - but don’t make it your first choice either.
Real Doctors, Real Choices
There’s disagreement among experts - and it’s messy.
Dr. Deepak Bhatt, who led major trials on clopidogrel, says the interaction is real and dangerous. He’s seen patients suffer stent clots after being put on omeprazole. In his practice, he switched his entire hospital system to pantoprazole.
On the other side, Dr. Marc Cohen, lead on the COGENT trial, argues the effect is too small to matter in practice. He’s never seen a clear case where the interaction caused harm. And he points out: if you skip the PPI, you risk a life-threatening GI bleed. For many, that’s a bigger threat.
Here’s what the data says about real-world use: a 2021 survey of over 1,200 cardiologists found 68% routinely prescribe PPIs with clopidogrel. But 42% chose pantoprazole as their first pick. That’s up from just 15% in 2010. Why? Because the evidence shifted.
Who Needs a PPI - And Who Doesn’t?
You don’t need a PPI just because you’re on clopidogrel. The American College of Gastroenterology says you need one only if you have two or more risk factors for bleeding:
- Age 65 or older
- History of ulcers or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Infected with H. pylori
- On high-dose aspirin or NSAIDs
If you have none of these? You probably don’t need a PPI at all. The risk of bleeding without one is low. The risk of a heart event from a bad PPI? That’s real.

What If You’re Already on Omeprazole?
If you’re currently taking omeprazole with clopidogrel, don’t stop either drug on your own. But do talk to your doctor.
Here’s what to ask:
- Do I have any GI risk factors that make a PPI necessary?
- Could I switch to pantoprazole?
- Is my clopidogrel working? Could I get tested for CYP2C19 variants?
If switching isn’t possible right away, some experts suggest staggering the doses: take your PPI in the morning and clopidogrel at night. This doesn’t eliminate the interaction, but it might reduce it by giving the enzymes time to recover.
The Bigger Picture: Cost, Genetics, and the Future
Pantoprazole costs about $1.27 per dose. Omeprazole? Around $0.38. That’s why some pharmacies still stock omeprazole - it’s cheaper. But when you factor in the cost of a heart attack or stent clot? The math changes.
Genetic testing for CYP2C19 is available. It costs $350-$500. It’s not for everyone. But if you’re young, have no GI risks, and are on clopidogrel - it might be worth it. If you’re a *2 carrier, you already have reduced clopidogrel response. Adding omeprazole? That’s doubling down on risk.
And the future? New drugs like ticagrelor don’t need CYP2C19 to work. They’re more effective and don’t interact with PPIs. But they cost over $500 a month. Clopidogrel is still the default because it’s cheap. That means this interaction isn’t going away.
Bottom Line: What You Should Do
- If you’re on clopidogrel and need a PPI, ask for pantoprazole - not omeprazole or esomeprazole.
- If you’re on omeprazole now, don’t panic - but talk to your doctor about switching.
- If you have no history of ulcers or GI bleeding, you may not need a PPI at all.
- Genetic testing can help if you’re high-risk or have had complications.
- Never stop clopidogrel without medical advice - the risk of clotting is immediate and deadly.
This isn’t about fear. It’s about smart choices. Your heart needs clopidogrel to work. Your stomach needs protection - but not at the cost of your life.
Can I take omeprazole with clopidogrel if I have a history of ulcers?
It’s not recommended. Omeprazole reduces clopidogrel’s effectiveness by up to 32%, increasing your risk of heart attack or stent clot. If you have a history of ulcers, pantoprazole is the safer choice - it protects your stomach without blocking clopidogrel. Ask your doctor to switch you.
Does pantoprazole completely eliminate the risk of interaction?
No interaction is completely eliminated, but pantoprazole has the weakest effect on CYP2C19 of all PPIs. Studies show it reduces clopidogrel’s active metabolite by only 14% at high doses - and often not at all at standard doses. It’s the safest PPI option for clopidogrel users.
Why do some doctors still prescribe omeprazole with clopidogrel?
Some doctors believe the clinical impact is too small to matter, especially if the patient has high GI bleeding risk. Others may not be aware of the latest guidelines. Cost is also a factor - omeprazole is cheaper. But current evidence and major guidelines clearly favor pantoprazole to avoid avoidable heart risks.
Can I take ranitidine instead of a PPI?
Ranitidine (Zantac) was once an alternative, but it was pulled from the U.S. market in 2020 due to contamination concerns. Other H2 blockers like famotidine are available and don’t interfere with clopidogrel. However, they’re less effective than PPIs at healing ulcers. For high-risk patients, pantoprazole is still preferred over H2 blockers.
Is genetic testing for CYP2C19 worth it?
For most people, no. But if you’ve had a stent clot despite taking clopidogrel, or if you’re under 60 with no GI risk factors, testing might help. About 30% of people carry a gene variant that makes clopidogrel less effective. If you’re one of them, avoiding omeprazole becomes even more critical. Testing costs $350-$500 and can guide long-term therapy.

Annie Joyce
February 13, 2026 AT 04:49Just had to comment because I’m a pharmacist and this is SO real. Saw a patient last month who had a stent clot after being on omeprazole for 'heartburn' - turns out she’d been on it for 3 years. Her cardiologist didn’t even know about the interaction. We switched her to pantoprazole and she’s been fine. Omeprazole is basically a silent killer here. Don’t let cheap meds cost you your life.
Rob Turner
February 14, 2026 AT 00:42man i just read this and my brain is like 🤯
so omeprazole is basically sabotaging my clopidogrel like a jealous ex? and pantoprazole is the chill friend who just says 'hey, i got you'?
also why is this not on every med bottle??
steve sunio
February 15, 2026 AT 01:07lol this whole post is overhyped. people are dying from PPIs now? next you’ll say water kills people if you drink too much. just stop taking the damn drug if you’re worried. also why is everyone acting like this is new info? been talking about this since 2012.
athmaja biju
February 15, 2026 AT 06:48India has been using pantoprazole as first-line for years. Why? Because we don’t waste money on dangerous generics. Americans think 'cheap' means 'smart' - no, it means 'dead'. This is why your healthcare system is broken. We save lives, you save pennies.
Robert Petersen
February 16, 2026 AT 07:05This is such a great breakdown - thank you for writing this. I’ve been on clopidogrel since my stent in 2020 and was on omeprazole until last year. My doc switched me to pantoprazole after reading this exact study. No more stomach issues, no heart scares. Just feels good to know you’re doing the right thing. Seriously, if you’re on this combo - talk to your doc. It’s a simple fix.
Craig Staszak
February 17, 2026 AT 23:52so here's the thing
if you're on clopidogrel and you have a history of bleeding
you probably need a ppi
but dont pick omeprazole
pantoprazole is the way
end of story
alex clo
February 18, 2026 AT 12:01The pharmacokinetic data supporting the interaction between omeprazole and clopidogrel is robust and reproducible across multiple randomized controlled trials. The clinical significance, however, remains debated due to confounding variables in observational studies. It is imperative that clinicians individualize therapy based on patient-specific risk factors rather than relying on blanket recommendations.
Joanne Tan
February 19, 2026 AT 13:46omg i just realized my mom is on omeprazole with her clopidogrel 😱
she’s 72, had a stent, and has zero ulcers
i’m calling her right now to tell her to ask her doctor about pantoprazole
thanks for this post!!
Carla McKinney
February 20, 2026 AT 05:00Everyone is acting like this is a revelation. But the FDA black box warning was issued in 2014. If you’re still using omeprazole with clopidogrel, you’re either negligent or misinformed. This isn’t a gray area. It’s a clear, evidence-based danger. Stop pretending it’s debatable.
Sonja Stoces
February 20, 2026 AT 15:41LOL why are we even talking about this? Just take ticagrelor already. It’s $500/month but at least you don’t have to play drug roulette. Also, why do we still have clopidogrel on formularies? It’s 2025. We’re still using 2008 meds because Big Pharma likes profits over patients. #PharmaGreed
Kristin Jarecki
February 22, 2026 AT 11:36This post provides a meticulously referenced, clinically grounded analysis of a critical drug interaction that has significant implications for cardiovascular and gastrointestinal outcomes. The distinction between CYP2C19-inhibiting and non-inhibiting proton pump inhibitors is not merely theoretical but has been validated through meta-analyses, randomized trials, and real-world data. The recommendation to prefer pantoprazole or dexlansoprazole over omeprazole or esomeprazole is consistent with current guidelines from the ACC, ESC, and ACG. Clinicians are ethically obligated to align prescribing practices with this evidence.
Jonathan Noe
February 23, 2026 AT 19:35Y’all are forgetting something - what about patients who can’t afford pantoprazole? It’s 3x the cost. Some of us are on Medicare with $10 copays for omeprazole. We’re not choosing this because we’re dumb - we’re choosing it because we’re poor. This isn’t just a medical issue. It’s a socioeconomic one. And nobody’s talking about that.
Jim Johnson
February 23, 2026 AT 22:00Just wanted to say - I’m a nurse and I’ve been pushing this exact info to my patients for years. One guy came in with a clot after his stent because he was on omeprazole for 'acid reflux' - he didn’t even know it was a problem. We got him switched to pantoprazole and he’s been fine. Don’t be shy - ask your doc. Bring this article. They’ll thank you later. You’re your own best advocate.